Initial Biological Assessment of Upconversion Nanohybrids
Abstract
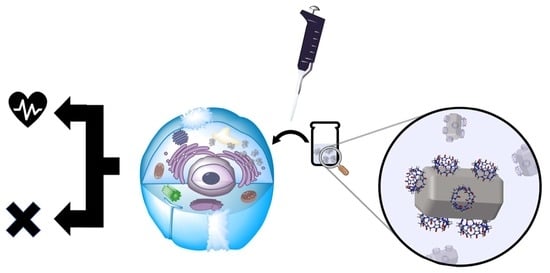
:1. Introduction
2. Materials and Methods
2.1. Chemicals
2.2. Synthesis NaYF4: Yb3+(20%), Er3+(2%) Nanoparticles (UCOA)
2.3. Synthesis of Bare NaYF4:Yb, Er UCNPs (UCn)
2.4. Functionalization of NaYF4:Yb, Er UCNPs with CB[7] (UC@CB[7])
2.5. Upconversion Luminescence (UCL) Measurements
2.6. High-Resolution Transmission Electron Microscopy (HRTEM)
2.7. Zeta Potential
2.8. Contamination with Bacteria and Endotoxin
2.9. Cell Exposures
2.10. Cellular Imaging
2.11. Dehydrogenase Activity (MTS) Assay
2.12. Lactate Dehydrogenase (LDH) Release
2.13. Cell Viability (MTT) Assay
2.14. Calcein-AM and Ethidium Homodimer-1 (EthD-1) Staining
3. Results
3.1. Synthesis of CB[7]-Capped UCNPs
3.2. Contamination with Bacteria/Endotoxin
3.3. Cytotoxicity
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Francés-Soriano, L.; González-Béjar, M.; Pérez-Prieto, J. Synergistic Effects in organic-coated upconversion nanoparticles. In Upconverting Nanomaterials: Perspectives, Synthesis, and Applications; Altavilla, C., Ed.; CRC Press: Boca Raton, FL, USA, 2016; pp. 101–138. ISBN 9781498707756. [Google Scholar]
- Li, Z.; Li, X.; Yang, Y.-W. Photoactive nanoparticles capped with macrocycles as platforms and hosts. In Micro and Nano Technologies; Pérez-Prieto, J., González-Béjar, M., Eds.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 139–167. ISBN 978-0-12-814531-9. [Google Scholar]
- Ramasamy, T.; Ruttala, H.B.; Gupta, B.; Poudel, B.K.; Choi, H.-G.; Yong, C.S.; Kim, J.O. Smart chemistry-based nanosized drug delivery systems for systemic applications: A comprehensive review. J. Control. Release 2017, 258, 226–253. [Google Scholar] [CrossRef]
- Ramasamy, T.; Munusamy, S.; Ruttala, H.B.; Kim, J.O. Smart Nanocarriers for the delivery of nucleic acid-based therapeutics: A comprehensive review. Biotechnol. J. 2021, 16, 1900408. [Google Scholar] [CrossRef] [PubMed]
- González-Béjar, M.; Francés-Soriano, L.; Pérez-Prieto, J. Upconversion nanoparticles for bioimaging and regenerative medicine. Front. Bioeng. Biotechnol. 2016, 4, 47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gnach, A.; Lipinski, T.; Bednarkiewicz, A.; Rybka, J.; Capobianco, J.A. Upconverting nanoparticles: Assessing the toxicity. Chem. Soc. Rev. 2015, 44, 1561–1584. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Qiu, H.; Prasad, P.N.; Chen, X. Upconversion nanoparticles: Design, nanochemistry, and applications in theranostics. Chem. Rev. 2014, 114, 5161–5214. [Google Scholar] [CrossRef]
- Li, Z.; Zhang, Y. An efficient and user-friendly method for the synthesis of hexagonal-phase NaYF4:Yb, Er/Tm nanocrystals with controllable shape and upconversion fluorescence. Nanotechnology 2008, 19, 345606. [Google Scholar] [CrossRef]
- Ma, C.; Bian, T.; Yang, S.; Liu, C.; Zhang, T.; Yang, J.; Li, Y.; Li, J.; Yang, R.; Tan, W. Fabrication of versatile cyclodextrin-functionalized upconversion luminescence nanoplatform for biomedical imaging. Anal. Chem. 2014, 86, 6508–6515. [Google Scholar] [CrossRef]
- Ding, Y.; Zhu, H.; Zhang, X.; Zhu, J.-J.; Burda, C. Rhodamine B derivative-functionalized upconversion nanoparticles for FRET-based Fe3+ sensing. Chem. Commun. 2013, 49, 7797–7799. [Google Scholar] [CrossRef] [Green Version]
- Maji, S.K.; Sreejith, S.; Joseph, J.; Lin, M.; He, T.; Tong, Y.; Sun, H.; Yu, S.W.-K.; Zhao, Y. Upconversion nanoparticles as a contrast agent for photoacoustic imaging in live mice. Adv. Mater. 2014, 26, 5633–5638. [Google Scholar] [CrossRef]
- Wang, A.; Jin, W.; Chen, E.; Zhou, J.; Zhou, L.; Wei, S. Drug delivery function of carboxymethyl-β-cyclodextrin modified upconversion nanoparticles for adamantine phthalocyanine and their NIR-triggered cancer treatment. Dalton Trans. 2016, 45, 3853–3862. [Google Scholar] [CrossRef]
- Wang, H.; Han, R.; Yang, L.; Shi, J.; Liu, Z.; Hu, Y.; Wang, Y.; Liu, S.; Gan, Y. Design and synthesis of core–shell–shell upconversion nanoparticles for NIR-induced drug release, photodynamic therapy, and cell imaging. ACS Appl. Mater. Interfaces 2016, 8, 4416–4423. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.; Yu, X.; Zhang, K.; Mirkin, C.A.; Li, J. Upconversion nanoprobes for the ratiometric luminescent sensing of nitric oxide. J. Am. Chem. Soc. 2017, 139, 12354–12357. [Google Scholar] [CrossRef] [PubMed]
- Montes-Navajas, P.; González-Béjar, M.; Scaiano, J.C.; García, H. Cucurbituril complexes cross the cell membrane. Photochem. Photobiol. Sci. 2009, 8, 1743–1747. [Google Scholar] [CrossRef]
- Lee, J.W.; Samal, S.; Selvapalam, N.; Kim, H.-J.; Kim, K. Cucurbituril homologues and derivatives: New opportunities in supramolecular chemistry. Acc. Chem. Res. 2003, 36, 621–630. [Google Scholar] [CrossRef] [PubMed]
- Lagona, J.; Mukhopadhyay, P.; Chakrabarti, S.; Isaacs, L. The Cucurbit[n]uril family. Angew. Chem. Int. Ed. 2005, 44, 4844–4870. [Google Scholar] [CrossRef] [PubMed]
- Wheate, N.J. Improving platinum(II)-based anticancer drug delivery using cucurbit[n]urils. J. Inorg. Biochem. 2008, 102, 2060–2066. [Google Scholar] [CrossRef]
- Jin Jeon, Y.; Kim, S.-Y.; Ho Ko, Y.; Sakamoto, S.; Yamaguchi, K.; Kim, K. Novel molecular drug carrier: Encapsulation of oxaliplatin in cucurbit[7]uril and its effects on stability and reactivity of the drug. Org. Biomol. Chem. 2005, 3, 2122–2125. [Google Scholar] [CrossRef] [Green Version]
- Sun, Y.; Zhang, W.; Wang, B.; Xu, X.; Chou, J.; Shimoni, O.; Ung, A.T.; Jin, D. A supramolecular self-assembly strategy for upconversion nanoparticle bioconjugation. Chem. Commun. 2018, 54, 3851–3854. [Google Scholar] [CrossRef] [Green Version]
- Francés-Soriano, L.; González-Béjar, M.; Pérez-Prieto, J. Cucurbit[n]uril-capped upconversion nanoparticles as highly emissive scaffolds for energy acceptors. Nanoscale 2015, 7, 5140–5146. [Google Scholar] [CrossRef] [Green Version]
- Oliveira, H.; Bednarkiewicz, A.; Falk, A.; Fröhlich, E.; Lisjak, D.; Prina-Mello, A.; Resch, S.; Schimpel, C.; Vrček, I.V.; Wysokińska, E.; et al. Critical considerations on the clinical translation of upconversion nanoparticles (UCNPs): Recommendations from the European Upconversion Network (COST Action CM1403). Adv. Healthcare Mater. 2019, 8, 1801233. [Google Scholar] [CrossRef] [Green Version]
- Dawson, M. Endotoxin limits for parenteral drug products. BET White Pap. 2017, 1, 1–7. [Google Scholar]
- Wysokińska, E.; Cichos, J.; Kowalczyk, A.; Karbowiak, M.; Strządała, L.; Bednarkiewicz, A.; Kałas, W. Toxicity mechanism of low doses of NaGdF4:Yb3+,Er3+ upconverting nanoparticles in activated macrophage cell lines. Biomolecules 2019, 9, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kembuan, C.; Oliveira, H.; Graf, C. Effect of different silica coatings on the toxicity of upconversion nanoparticles on RAW 264.7 macrophage cells. Beilstein J. Nanotechnol. 2021, 12, 35–48. [Google Scholar] [CrossRef] [PubMed]
- Bogdan, N.; Vetrone, F.; Ozin, G.A.; Capobianco, J.A. Synthesis of ligand-free colloidally stable water dispersible brightly luminescent lanthanide-doped upconverting nanoparticles. Nano Lett. 2011, 11, 835–840. [Google Scholar] [CrossRef]
- Edgell, C.J.; McDonald, C.C.; Graham, J.B. Permanent cell line expressing human factor VIII-related antigen established by hybridization. Proc. Natl. Acad. Sci. USA 1983, 80, 3734–3737. [Google Scholar] [CrossRef] [Green Version]
- Fröhlich, E.; Meindl, C.; Wagner, K.; Leitinger, G.; Roblegg, E. Use of whole genome expression analysis in the toxicity screening of nanoparticles. Toxicol. Appl. Pharmacol. 2014, 280, 272–284. [Google Scholar] [CrossRef] [Green Version]
- Ferrera-González, J.; Francés-Soriano, L.; Estébanez, N.; Navarro-Raga, E.; González-Béjar, M.; Pérez-Prieto, J. NIR laser scanning microscopy for photophysical characterization of upconversion nanoparticles and nanohybrids. Nanoscale 2021, 13, 10067–10080. [Google Scholar] [CrossRef]
- Palma, P.F.R.; Baggio, G.L.; Spada, C.; Silva, R.; da Ferreira, S.I.A.C.P.; Treitinger, A. Evaluation of annexin V and Calcein-AM as markers of mononuclear cell apoptosis during human immunodeficiency virus infection. Braz. J. Infect. Dis. 2008, 12, 108–114. [Google Scholar] [CrossRef] [Green Version]
- Lahtinen, S.; Lyytikäinen, A.; Päkkilä, H.; Hömppi, E.; Perälä, N.; Lastusaari, M.; Soukka, T. Disintegration of hexagonal NaYF4:Yb3+,Er3+ upconverting nanoparticles in aqueous media: The role of fluoride in solubility equilibrium. J. Phys. Chem. C 2017, 121, 656–665. [Google Scholar] [CrossRef]
- Estebanez, N.; González-Béjar, M.; Pérez-Prieto, J. Polysulfonate cappings on upconversion nanoparticles prevent their disintegration in water and provide superior stability in a highly acidic medium. ACS Omega 2019, 4, 3012–3019. [Google Scholar] [CrossRef] [Green Version]
- Kirchner, D.; Henwood, S. Toxicity and safety testing. In The Laboratory Rabbit, Guinea Pig, Hamster, and Other Rodents; Academic Press: Cambridge, MA, USA, 2012; pp. 275–300. ISBN 9780123809209. [Google Scholar]
- Karlsson, H.L.; Cronholm, P.; Gustafsson, J.; Möller, L. Copper oxide nanoparticles are highly toxic: A comparison between metal oxide nanoparticles and carbon nanotubes. Chem. Res. Toxicol. 2008, 21, 1726–1732. [Google Scholar] [CrossRef]
- Fröhlich, E.; Meindl, C.; Pieber, T.R. Important issues in the cytotoxicity screening of nano-sized materials. EURO-NanoTox-Lett. 2015, 2, 1–5. [Google Scholar] [CrossRef] [Green Version]
- International Organization for Standardization. Biological Evaluation of Medical Devices—Part 5: Tests for In Vitro Cytotoxicity; ISO 10993-5; ISO: Geneva, Switzerland, 2019. [Google Scholar]
- Fröhlich, E. The role of surface charge in cellular uptake and cytotoxicity of medical nanoparticles. Int. J. Nanomed. 2012, 7, 5577–5591. [Google Scholar] [CrossRef] [Green Version]
- Akter, F.; Ponnaiyan, S.; Kögler-Mohrbacher, B.; Bleibaum, F.; Damme, M.; Renard, B.Y.; Winter, D. Multi cell line analysis of lysosomal proteomes reveals unique features and novel lysosomal proteins. bioRxiv 2020, 423747. [Google Scholar] [CrossRef]
- Günther, J.; Seyfert, H.-M. The first line of defence: Insights into mechanisms and relevance of phagocytosis in epithelial cells. Semin. Immunopathol. 2018, 40, 555–565. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Assaf, K.I.; Nau, W.M. Cucurbiturils: From synthesis to high-affinity binding and catalysis. Chem. Soc. Rev. 2015, 44, 394–418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pennakalathil, J.; Jahja, E.; Özdemir, E.S.; Konu, Ö.; Tuncel, D. Red emitting, cucurbituril-capped, pH-responsive conjugated oligomer-based nanoparticles for drug delivery and cellular imaging. Biomacromolecules 2014, 15, 3366–3374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Özkan, M.; Hadi, S.E.; Tunç, İ.; Midilli, Y.; Ortaç, B.; Tuncel, D. Cucurbit[7]uril-capped hybrid conjugated oligomer-gold nanoparticles for combined photodynamic-photothermal therapy and cellular imaging. ACS Appl. Polym. Mater. 2020, 2, 3840–3849. [Google Scholar] [CrossRef]
- Francés-Soriano, L.; Peruffo, N.; Natile, M.M.; Hildebrandt, N. Er3+-to-dye energy transfer in DNA-coated core and core/shell/shell upconverting nanoparticles with 980 nm and 808 nm excitation of Yb3+ and Nd3+. Analyst 2020, 145, 2543–2553. [Google Scholar] [CrossRef]
- Verma, A.; Ali, D.; Pathak, A.K. Fluoride induces DNA damage and cytotoxicity in human hepatocellular carcinoma cells. Toxicol. Environ. Chem. 2017, 99, 148–159. [Google Scholar] [CrossRef]
- Gautom, K.D.; Stark, D.T.; Kennedy, I.M. Potential toxicity of up-converting nanoparticles encapsulated with a bilayer formed by ligand attraction. Langmuir 2014, 30, 8167–8176. [Google Scholar] [CrossRef] [Green Version]
- Saleh, M.I.; Rühle, B.; Wang, S.; Radnik, J.; You, Y.; Resch-Genger, U. Assessing the protective effects of different surface coatings on NaYF4:Yb3+, Er3+ upconverting nanoparticles in buffer and DMEM. Sci. Rep. 2020, 10, 19318. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Yin, W.; Peng, T.; Chang, Y.; Zu, Y.; Li, J.; He, X.; Ma, X.; Gu, Z.; Zhao, Y. Biodistribution, excretion, and toxicity of polyethyleneimine modified NaYF4:Yb,Er upconversion nanoparticles in mice via different administration routes. Nanoscale 2017, 9, 4497–4507. [Google Scholar] [CrossRef] [PubMed]
- Krug, H.F. Nanosafety research—are we on the right track? Angew. Chem. Int. Ed. 2014, 53, 12304–12319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fröhlich, E. Cellular targets and mechanisms in the cytotoxic action of non-biodegradable engineered nanoparticles. Curr. Drug Metab. 2013, 14, 976–988. [Google Scholar] [CrossRef] [PubMed]






| Nanomaterial | Concentration/μg/mL | Clot Test 1 1 | Clot Test 2 1 |
|---|---|---|---|
| UCn | 200 | - | - |
| 20 | - | - | |
| 2 | - | - | |
| 5 | - | - | |
| UC@CB[7] | 200 | - | - |
| 20 | - | - | |
| 2 | - | - | |
| 5 | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferrera-González, J.; Francés-Soriano, L.; Galiana-Roselló, C.; González-Garcia, J.; González-Béjar, M.; Fröhlich, E.; Pérez-Prieto, J. Initial Biological Assessment of Upconversion Nanohybrids. Biomedicines 2021, 9, 1419. https://doi.org/10.3390/biomedicines9101419
Ferrera-González J, Francés-Soriano L, Galiana-Roselló C, González-Garcia J, González-Béjar M, Fröhlich E, Pérez-Prieto J. Initial Biological Assessment of Upconversion Nanohybrids. Biomedicines. 2021; 9(10):1419. https://doi.org/10.3390/biomedicines9101419
Chicago/Turabian StyleFerrera-González, Juan, Laura Francés-Soriano, Cristina Galiana-Roselló, Jorge González-Garcia, María González-Béjar, Eleonore Fröhlich, and Julia Pérez-Prieto. 2021. "Initial Biological Assessment of Upconversion Nanohybrids" Biomedicines 9, no. 10: 1419. https://doi.org/10.3390/biomedicines9101419
APA StyleFerrera-González, J., Francés-Soriano, L., Galiana-Roselló, C., González-Garcia, J., González-Béjar, M., Fröhlich, E., & Pérez-Prieto, J. (2021). Initial Biological Assessment of Upconversion Nanohybrids. Biomedicines, 9(10), 1419. https://doi.org/10.3390/biomedicines9101419