Classifying Maxillary Sinuses of Polish Patients for Sinus Lift: A Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
- An edentulous area in the posterior maxilla with a potential sinus floor augmentation;
- No radiological signs of maxillary sinus disease (i.e., a widened Schneiderian membrane, radiological image typical of chronic sinusitis, foreign bodies);
- No history of a direct osteotomy (e.g., osteotomy to remove a foreign body from the maxillary sinus);
- The last tooth extraction or other surgical intervention in the posterior maxilla was performed no earlier than 12 months ago at the time of data collection.
- Sub-sinus residual bone height: measured as the distance from the top of the alveolar ridge to the floor of the sinus to establish whether sinus floor augmentation is necessary before implant placement.
- Thickness of the lateral wall: measured on the level of assumed window osteotomy, at the thinnest point.
- Thickness of the palatal wall: measured in the middle of the wall, also at the thinnest point.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Balaji, S.M. Direct v/s Indirect sinus lift in maxillary dental implants. Ann. Maxillofac. Surg. 2013, 3, 148–153. [Google Scholar] [CrossRef]
- Cavalcanti, M.C.; Guirado, T.E.; Sapata, V.M.; Costa, C.; Pannuti, C.M.; Jung, R.E.; Neto, J.B.C. Maxillary sinus floor pneumatization and alveolar ridge resorption after tooth loss: A cross-sectional study. Braz. Oral Res. 2018, 32, e64. [Google Scholar] [CrossRef]
- Pjetursson, B.E.; Tan, W.C.; Zwahlen, M.; Lang, N.P. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. Part I: Lateral approach. J. Clin. Periodontol. 2008, 35 (Suppl. 8), 216–240. [Google Scholar] [CrossRef] [PubMed]
- Summers, R.B. A new concept in maxillary implant surgery: The osteotome technique. Compendium 1994, 15, 152, 154–156, 158 passim; quiz 162. [Google Scholar]
- Taschieri, S.; Del Fabbro, M.; Tsesis, I.; Corbella, S. Maxillary Sinus in relation to Modern Oral and Maxillofacial Surgery. Int. J. Dent. 2012, 2012, 391012. [Google Scholar] [CrossRef]
- Caudry, S.; Landzberg, M. Lateral window sinus elevation technique: Managing challenges and complications. J. Can. Dent. Assoc. 2013, 79, d101. [Google Scholar]
- Raja, S.V. Management of the posterior maxilla with sinus lift: Review of techniques. J. Oral Maxillofac. Surg. 2009, 67, 1730–1734. [Google Scholar] [CrossRef] [PubMed]
- Smiler, D.G.; Johnson, P.W.; Lozada, J.L.; Misch, C.; Rosenlicht, J.L.; Tatum, O.H., Jr.; Wagner, J.R. Sinus lift grafts and endosseous implants. Treatment of the atrophic posterior maxilla. Dent. Clin. N. Am. 1992, 36, 151–186, discussion 187. [Google Scholar] [CrossRef]
- Timmenga, N.M.; Raghoebar, G.M.; van Weissenbruch, R.; Vissink, A. Maxillary sinusitis after augmentation of the maxillary sinus floor: A report of 2 cases. J. Oral Maxillofac. Surg. 2001, 59, 200–204. [Google Scholar] [CrossRef]
- Jensen, O.T.; Perkins, S.; Van de Water, F.W. Nasal fossa and maxillary sinus grafting of implants from a palatal approach: Report of a case. J. Oral Maxillofac. Surg. 1992, 50, 415–418. [Google Scholar] [CrossRef]
- Stübinger, S.; Saldamli, B.; Seitz, O.; Sader, R.; Landes, C.A. Palatal versus vestibular piezoelectric window osteotomy for maxillary sinus elevation: A comparative clinical study of two surgical techniques. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 107, 648–655. [Google Scholar] [CrossRef] [PubMed]
- Stübinger, S.; Saldamli, B.; Landes, C.A.; Sader, R. Palatal piezosurgical window osteotomy for maxillary sinus augmentation. Int. J. Oral Maxillofac. Surg. 2010, 39, 606–609. [Google Scholar] [CrossRef]
- Seemann, R.; Wagner, F.; Ewers, R.; Ulm, C. Palatal sinus elevation revisited: A technical note. J. Oral Maxillofac. Surg. 2013, 71, 1347–1352. [Google Scholar] [CrossRef]
- Soardi, C.M.; Wang, H.-L. New crestal approach for lifting sinus in the extremely atrophic upper maxillae. Clin. Adv. Periodontics 2012, 2, 179–185. [Google Scholar] [CrossRef]
- Rahpeyma, A.; Khajehahmadi, S. Indications for palatal sinus lift: Case series. J. Indian Soc. Periodontol. 2018, 22, 254–256. [Google Scholar] [CrossRef]
- Ueno, D.; Kurokawa, T.; Maruo, K.; Watanabe, T.; Jayawardena, J.A. Palatal window osteotomy technique improves maxillary sinus augmentation in previously insufficient augmentation case. Int. J. Implant Dent. 2015, 1, 19. [Google Scholar] [CrossRef]
- Yin, S.; Tarnow, D.; Wallace, S.S. Remediation of a failed lateral window sinus augmentation via a palatal approach: Rationale and case report. Int. J. Periodontics Restor. Dent. 2022, 42, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Gracco, A.; Luca, L.; Cozzani, M.; Siciliani, G. Assessment of palatal bone thickness in adults with cone beam computerised tomography. Aust. Orthod. J. 2007, 23, 109–113. [Google Scholar] [CrossRef]
- Tavelli, L.; Borgonovo, A.E.; Re, D.; Maiorana, C. Sinus presurgical evaluation: A literature review and a new classification proposal. Minerva Stomatol. 2017, 66, 115–131. [Google Scholar] [CrossRef]
- Starch-Jensen, T.; Jensen, J.D. Maxillary sinus floor augmentation: A review of selected treatment modalities. J. Oral Maxillofac. Res. 2017, 8, e3. [Google Scholar] [CrossRef]
- Richardson, G.; Russell, K.A. A review of impacted permanent maxillary cuspids—Diagnosis and prevention. J. Can. Dent. Assoc. 2000, 66, 497–501. [Google Scholar] [PubMed]
- Wagner, F.; Dvorak, G.; Nemec, S.; Pietschmann, P.; Traxler, H.; Schicho, K.; Seemann, R. Morphometric analysis of sinus depth in the posterior maxilla and proposal of a novel classification. Sci. Rep. 2017, 7, 45397. [Google Scholar] [CrossRef] [PubMed]
- Wagner, F.; Dvorak, G.; Pillerstorff, R.; Traxler, H.; Nemec, S.; Pietschmann, P.; Seemann, R. Anatomical preconditions for the palatal sinus floor augmentation—A three-dimensional feasibility study. J. Craniomaxillofac. Surg. 2015, 43, 1303–1308. [Google Scholar] [CrossRef] [PubMed]



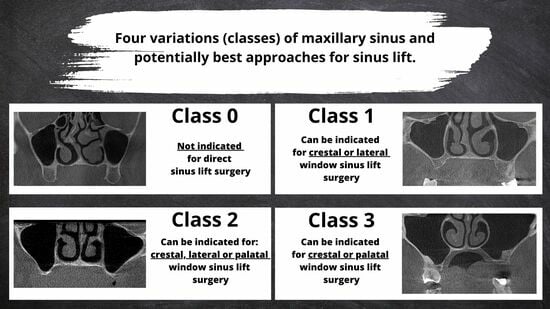
| Class | 0 | 1 | 2 | 3 |
|---|---|---|---|---|
| Incidence Rate | 4% | 44% | 49% | 3% |
| Sinus Lifting Procedure | Not indicated for direct sinus lift surgery | Can be indicated for crestal or lateral window sinus lift surgery | Can be indicated for crestal, lateral, or palatal window sinus lift surgery | Can be indicated for crestal or palatal window sinus lift surgery |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jadach, R.; Asa’ad, F.; Rasperini, G.; Osypko, K. Classifying Maxillary Sinuses of Polish Patients for Sinus Lift: A Pilot Study. Dent. J. 2024, 12, 35. https://doi.org/10.3390/dj12020035
Jadach R, Asa’ad F, Rasperini G, Osypko K. Classifying Maxillary Sinuses of Polish Patients for Sinus Lift: A Pilot Study. Dentistry Journal. 2024; 12(2):35. https://doi.org/10.3390/dj12020035
Chicago/Turabian StyleJadach, Radosław, Farah Asa’ad, Giulio Rasperini, and Karolina Osypko. 2024. "Classifying Maxillary Sinuses of Polish Patients for Sinus Lift: A Pilot Study" Dentistry Journal 12, no. 2: 35. https://doi.org/10.3390/dj12020035
APA StyleJadach, R., Asa’ad, F., Rasperini, G., & Osypko, K. (2024). Classifying Maxillary Sinuses of Polish Patients for Sinus Lift: A Pilot Study. Dentistry Journal, 12(2), 35. https://doi.org/10.3390/dj12020035