Editorial Board Members’ Collection Series: Contemporary Perioperative Concepts in Cancer Surgery
A topical collection in Current Oncology (ISSN 1718-7729). This collection belongs to the section "Surgical Oncology".
Viewed by 41413Editors
Interests: patient safety during anesthesia; the use of AI in postoperative recovery (PACU); optimization of anesthesia pharmacology through predictive analytics; enhancing perioperative workflows using AI-driven tools
Special Issues, Collections and Topics in MDPI journals
Interests: abdominal surgery; radiation therapy; anesthesiology; hepatobiliary and pancreatic surgery
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
Cancer is a major global public health concern that affects all communities across the world. Globally, the incidence of cancer is predicted to increase by 50% by the year 2030; and during the same period, cancer-related mortality is projected to increase by 60% to 13.1 million deaths worldwide. This increasing trend in cancer-related mortality is mainly due to the increasing incidence of cancer and cancer-related mortality in the developing world and the overall increase in global population, particularly the marked increase in the population over the age of 60 years.
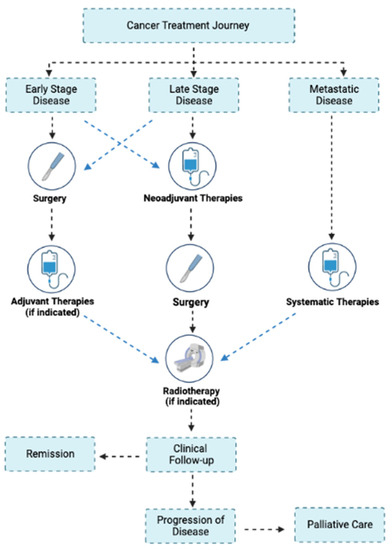
Of the nearly 20 million new cancer cases worldwide in 2022, over 80% of cases will need surgery, some several times, as curative resection is essential for cancer control, particularly for those with solid tumors. Given the emerging tsunami of cancer and increasing need for surgical cancer care; understanding advances in cancer biology, rapidly evolving cancer therapeutics, modern surgical techniques, and evolving patient-centered, recovery-focused perioperative care concepts is essential for anesthesiologists, perioperative clinicians, surgeons, nurses, intensivists, pain medicine clinicians and integrative medicine specialists.
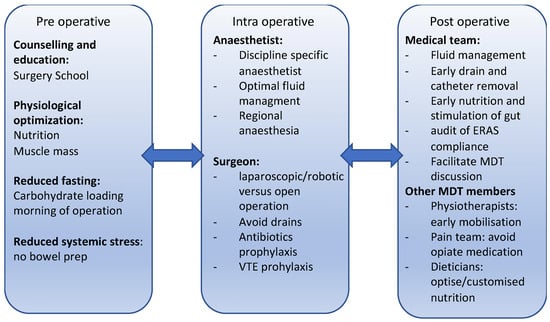
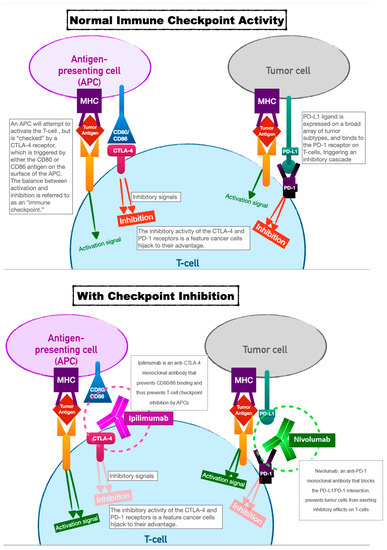
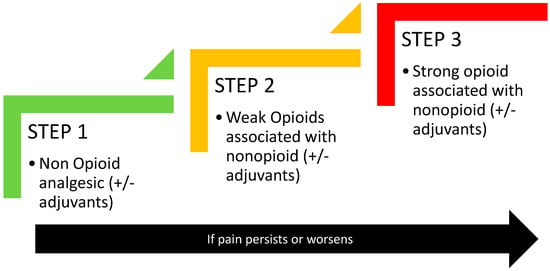
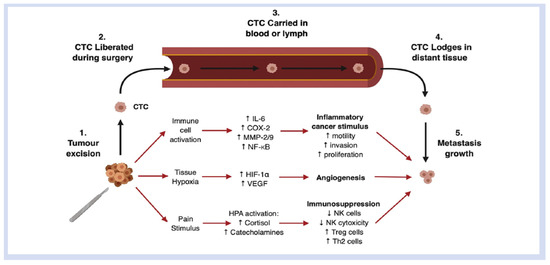
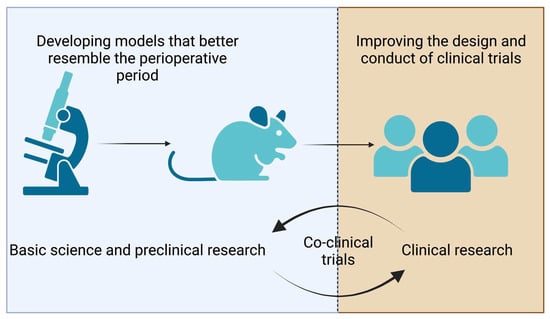
The perioperative period is a pathophysiological state characterized by intense emotional and physiological (surgical) stress, pain, inflammation, immune suppression, negative nitrogen balance, and insulin resistance. The combined effect of neuro-inflammatory signaling and endocrine-metabolic effects in the perioperative period can lead to immune suppression and altered immune responses, influencing wound healing and recovery from surgery. However, these pathways are also an integral component of the inflammatory-immune responses leading to an immunosuppressive microenvironment in tumor stromal tissue, particularly in the presence of postoperative complications. Our understanding of perioperative factors that contribute to tumor spread and recurrence (from minimal residual disease, circulating tumor cells, or micro metastatic disease) is rapidly evolving with the potential to influence long-term cancer outcomes. In the surgical cancer patient, effective perioperative strategies and surgical techniques should, therefore, not only aim to provide effective analgesia and control of symptom burden, but also aim for margin free resection, minimize preventable complications and enhance functional recovery. Surgical techniques, operative approaches, and perioperative cancer therapies should also aim to attenuate the surgical stress response and positively modulate the inflammatory-immune response for improved clinical, oncological, and patient-centered outcomes.
This Topical Collection of Current Oncology titled “Contemporary Perioperative Concepts in Cancer Surgery” will address key topics of advances in cancer biology, newer cancer therapeutics, modern surgical techniques, and evolving patient-centered, recovery-focused perioperative care concepts that directly influence patient outcomes. Each of the articles is authored by international experts in the field and discusses the current understanding and practices, ongoing controversies and unanswered questions, and the direction for future studies. This exercise, we hope, will highlight the need for ongoing scientific study on key areas to further enhance perioperative and periprocedural care of our patients with cancer and cancer survivors.
Sincerely,
Prof. Dr. Vijaya Gottumukkala
Prof. Dr. Jörg Kleeff
Collection Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Current Oncology is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2200 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- advances in cancer biology
- modern surgical techniques
- perioperative care
- anesthetic technique
- pain management
- rehabilitative and palliative care