Advances in Coronary Heart Disease
A topical collection in Life (ISSN 2075-1729). This collection belongs to the section "Medical Research".
Viewed by 48353Editor
Interests: acute coronary syndrome; coronary microvascular dysfunction; chronic coronary syndrome; microvascular spasm; percutaneous coronary intervention; vasospastic angina
Topical Collection Information
Dear Colleagues,
As you know, guidelines and other preventive measures for coronary heart disease (CHD) have been reworked and made more practical. Nonetheless, CHD remains an essential component of cardiovascular disease and can cause acute and chronic coronary syndromes, heart failure, fatal arrhythmias and sudden cardiac death.
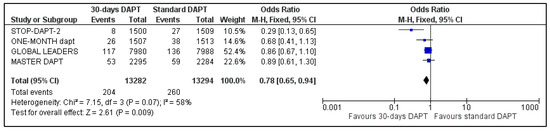
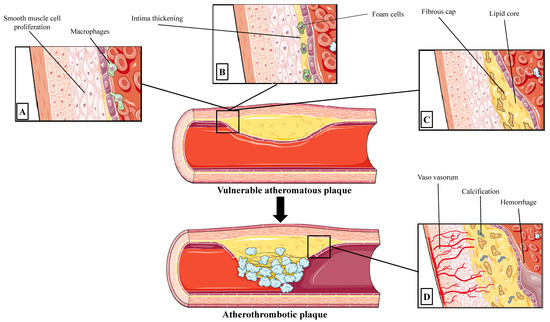
In acute coronary syndrome (ACS), there is no disagreement with the policy of considering early revascularisation for ST-elevation myocardial infarction (STEMI) and coronary angiography and revascularisation for non-ST elevation ACS risk assessment. However, many items remain unresolved, including the need for the re-evaluation of aspiration thrombectomy in STEMI patients and the usefulness of recent heart failure drugs for ACS.
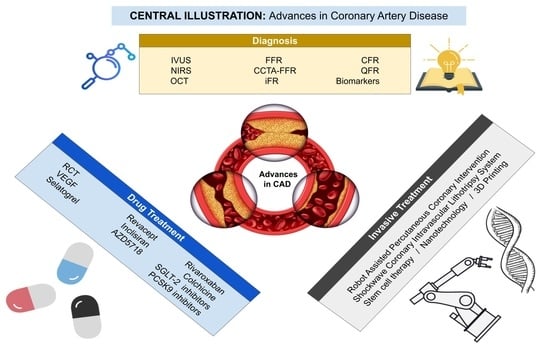
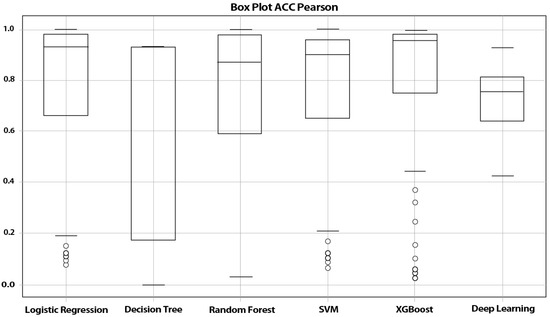
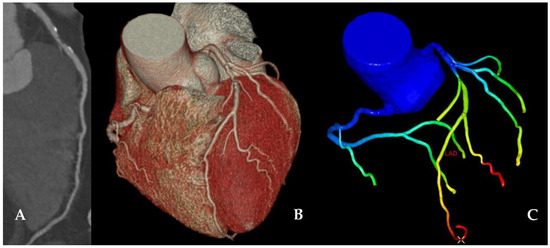
Some impactful studies have recently shown that revascularisation does not have the same predictive value as optimal medical therapy in stable chronic coronary syndrome (CCS), indicating the need to reconsider CCS treatment. The incidence of procedure-related myocardial infarction has been identified as a substantial complication. Preventing such an occurrence is becoming increasingly crucial in revascularisation, with an emphasis on ischemia diagnosis and safe revascularisation. Current diagnostic methods for myocardial ischemia include imaging and functional diagnosis, which can be non-invasive or invasive. In addition, artificial intelligence is being used in some imaging diagnostics.
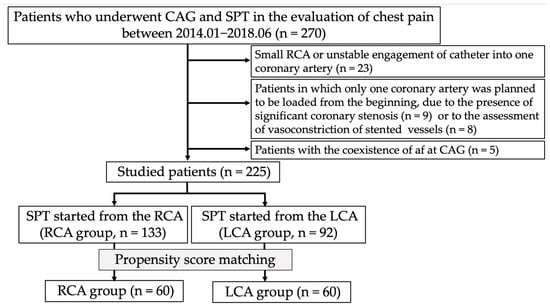
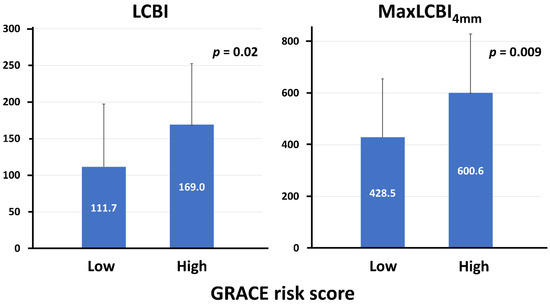
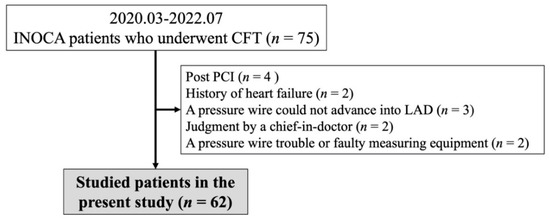
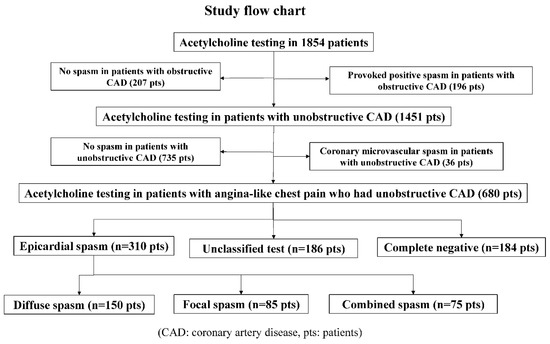
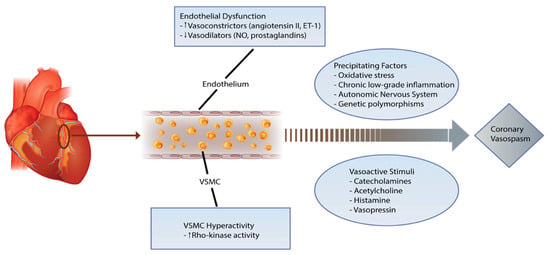
Furthermore, ischemic heart disease without organic stenosis is known as myocardial infarction with nonobstructive coronary arteries (MINOCA) or ischemia with nonobstructive coronary arteries (INOCA). Coronary artery dysfunctions, including vasospastic angina, microvascular spasm and coronary microvascular dysfunction (CMD), are now widely considered the primary pathophysiology of such diseases, and guidelines directly address them. The invasive and non-invasive diagnoses of coronary artery dysfunction have been the subject of much debate. Presently, there is no clear consensus on which methods and protocols are superior and better. Moreover, despite recent guidelines, describing the treatment of these coronary artery dysfunctions, particularly those resulting in abnormal resistance vessels, the actual clinical situation is still chaotic, and many patients appear to be changing drugs manually.
In this Topical Collection of ‘Advances in Coronary Heart Disease’, we have compiled the latest information on ACS and CCS diagnoses, treatment and prognosis, including clinical studies and reviews, to provide the current knowledge on these diseases.
Dr. Hiroki Teragawa
Collection Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Life is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2600 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- acute coronary syndrome
- chronic coronary syndrome
- ischemia with no obstructive coronary arteries
- vasospastic angina
- microvascular spasm
- coronary microvascular dysfunction