Dietary Fatty Acids and the Cardiovascular Health: Evidence, Controversies, and Consensus
A topical collection in Nutrients (ISSN 2072-6643). This collection belongs to the section "Lipids".
Viewed by 20218Editor
Interests: lipids and brain development; fatty acid uptake system in human placenta; angiogenesis; feto-placental growth and development; DHA and cell growth and proliferation; lipid nutrition; eicosanoids; cardiovascular health; platelet function
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
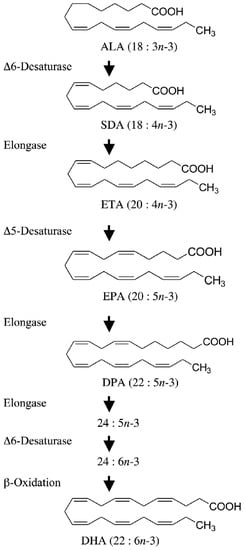
Fatty acids play vital roles in the cardiovascular system via several mechanisms. Impacts of dietary fatty acids on the cardiovascular system depend on their structure, metabolism, and bioactivity. In addition to affecting plasma lipids such as plasma cholesterols, triglycerides, and free fatty acids, dietary fatty acids may also affect the risk of cardiovascular disease (CVD) through their effects on inflammation, endothelial function, thrombosis, ventricular arrhythmias, and blood pressure.
The current recommendation on dietary fat intake is to reduce total fat consumption and use healthier unsaturated fatty acids instead of harmful saturated fatty acids. Nevertheless, some have questioned the scientific evidence underlying current and previous dietary advice. Animal fats are the primary source of saturated fats in many modern diets. However, some animal fats are higher in monounsaturated fats than saturated fats. In addition, polyunsaturated fats in vegetable oils will typically contain omega (n)-3, 6, and 9 fatty acids in different concentrations. Another significant criticism is that different fats never occur alone in the diet but always co-exist in several foodstuffs. Hence, conclusions about the health effects of saturated and polyunsaturated fatty acids are unlikely to consistently translate to the health effects of fats, oils, and foods in which those fatty acids are present. This is presumably one of the reasons for the many discordant results from observational studies. These open issues therefore welcome all sorts of research on fatty acid involving fatty acids such as on CVD risk factors, metabolic syndrome, epidemiological and mechanistic studies, reviews, plant oils, saturated and PUFAs.
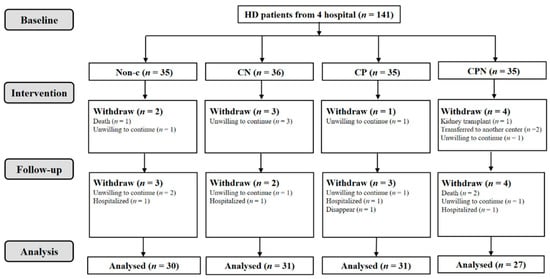
The objective of this Topical Collection on “Dietary Fatty Acids and Cardiovascular Health: Evidence, Controversies, and Consensus” is to showcase the latest research focusing on the impact of dietary fatty acids, metabolic diseases, diabetes, platelet function, blood coagulation, mechanistic studies, and lipid profile status, as well as intervention studies with fatty acids’ CVD outcome.
This Topical Collection is intended to provide a contemporary summary of current knowledge while providing guidance for future research in the field.
Prof. Dr. Asim K. Duttaroy
Collection Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Nutrients is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2900 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- fatty acids
- cardiovascular disease
- cardiovascular health
- saturated fatty acids
- PUFAs
- metabolic syndrome
- epidemiology