Release of Antibiotics Out of a Moldable Collagen-β-Tricalciumphosphate-Composite Compared to Two Calcium Phosphate Granules
Abstract
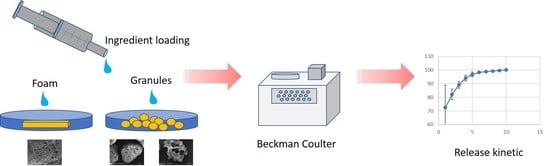
:1. Introduction
2. Materials and Methods
2.1. Drug Eluting Matrices
2.2. SEM Examination and Materials Characterization
2.3. Antibiotics Measurement Assay
2.4. Antibiotics Uptake Preparation
2.5. Measurement of Total Antibiotics Uptake
2.6. Measurement of the Release Kinetics
2.7. Statistical Methods
3. Results
3.1. SEM Examination
3.2. Antibiotics Uptake
3.3. Antibiotic Release in Aqueous Solution
3.4. Inhibition Zones
3.4.1. Staphylococcus Aureus
3.4.2. Bacillus Subtilis
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Maier, G.S.; Roth, K.E.; Andereya, S.; Birnbaum, K.; Niedhart, C.; Lühmann, M.; Ohnsorge, J.; Maus, U. In vitro elution characteristics of gentamicin and vancomycin from synthetic bone graft substitutes. Open Orthop. J. 2013, 7, 624–629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khoshzaban, A.; Mehrzad, S.; Tavakoli, V.; Keshel, S.H.; Behrouzi, G.R.; Bashtar, M. The comparative effectiveness of demineralized bone matrix, beta-tricalcium phosphate, and bovine-derived anorganic bone matrix on inflammation and bone formation using a paired calvarial defect model in rats. Clin. Cosmet. Investig. Dent. 2011, 3, 69–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bernhardt, A.; Lode, A.; Peters, F.; Gelinsky, M. Comparative evaluation of different calcium phosphate-based bone graft granules—An in vitro study with osteoblast-like cells. Clin. Oral. Implant. Res. 2013, 24, 441–449. [Google Scholar] [CrossRef] [PubMed]
- Elliott, J.C. Structure and Chemistry of the Apatites and Other Calcium Orthophosphates; Studies in Inorganic Chemistry 18; Elsevier: Amsterdam, The Netherlands, 1994. [Google Scholar]
- Daculsi, G.; Uzel, A.P.; Weiss, P.; Goyenvalle, E.; Aguado, E. Developments in injectable multiphasic biomaterials. The performance of microporous biphasic calcium phosphate granules and hydrogels. J. Mater. Sci. Mater. Med. 2010, 21, 855–861. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rothamel, D.; Schwarz, F.; Sager, M.; Herten, M.; Sculean, A.; Becker, J. Biodegradation of differently cross-linked collagen membranes: An experimental study in the rat. Clin. Oral. Implant. Res. 2005, 16, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; Rothamel, D.; Herten, M.; Sager, M.; Becker, J. Angiogenesis pattern of native and cross-linked collagen membranes: An immunohistochemical study in the rat. Clin. Oral. Implant. Res. 2006, 17, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Harle, A.; Ritzerfeld, J. The release of gentamycin into the wound secretions from polymethylmethacrylate beads. A study with reference to the animal experiment. Arch. Orthop. Trauma. Surg. 1979, 95, 65–70. [Google Scholar] [CrossRef]
- Caplin, J.D.; Garcia, A.J. Implantable antimicrobial biomaterials for local drug delivery in bone infection models. Acta Biomater. 2019, 93, 2–11. [Google Scholar] [CrossRef]
- Boelch, S.P.; Rueckl, K.; Fuchs, C.; Jordan, M.; Knauer, M.; Steiert, A.; Rudert, M.; Luedemann, M. Comparison of Elution Characteristics and Compressive Strength of Biantibiotic-Loaded PMMA Bone Cement for Spacers: Copal® Spacem with Gentamicin and Vaoncomycin versus Palacos® R+G with Vancomycin. Biomed Res. Int. 2018, 4323518. [Google Scholar] [CrossRef] [Green Version]
- Springer, B.D.; Lee, G.C.; Osmon, D.; Haidukewych, G.J.; Hanssen, A.D.; Jacofsky, D.J. Systemic safety of high-dose antibiotic-loaded cement spacers after resection of an infected total knee arthroplasty. Clin. Orthop. Relat. Res. 2004, 427, 47–51. [Google Scholar] [CrossRef]
- Fink, B.; Vogt, S.; Reinsch, M.; Büchner, H. Sufficient release of antibiotic by a spacer 6 weeks after implantation in two-stage revision of infected hip prostheses. Clin. Orthop. Relat. Res. 2011, 469, 3141–3147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nelson, C.L.; Griffin, F.M.; Harrison, B.H.; Cooper, R.E. In vitro elution characteristics of commercially and noncommercially prepared antibiotic PMMA beads. Clin. Orthop. Relat. Res. 1992, 284, 303–309. [Google Scholar] [CrossRef]
- Marques, C.; Tasse, J.; Pracros, A.; Collin, V.; Franceschi, C.; Laurent, F.; Chatellier, S.; Forestier, C. Effects of antibiotics on biofilm and unattached cells of a clinical Staphylococcus aureus isolate from bone and joint infection. J. Med. Microbiol. 2015, 64, 1021–1026. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van de Belt, H.; Neut, D.; Schenk, W.; van Horn, J.R.; van der Mei, H.C.; Busscher, H.J. Gentamicin release from polymethylmethacrylate bone cements and Staphylococcus aureus biofilm formation. Acta Orthop. Scand. 2000, 71, 625–629. [Google Scholar] [CrossRef]
- McKee, M.D.; Li-Bland, E.A.; Wild, L.M.; Schemitsch, E.H. A prospective, randomized clinical trial comparing an antibiotic-impregnated bioabsorbable bone substitute with standard antibiotic-impregnated cement beads in the treatment of chronic osteomyelitis and infected nonunion. J. Orthop. Trauma. 2010, 24, 483–490. [Google Scholar] [CrossRef]
- Gitelis, S.; Piasecki, P.; Turner, T.; Haggard, W.; Charters, J.; Urban, R. Use of a calcium sulfate-based bone graft substitute for benign bone lesions. Orthopedics 2001, 24, 162–166. [Google Scholar]
- Shiramizu, K.; Lovric, V.; Leung, A.; Walsh, W.R. How do porosity-inducing techniques affect antibiotic elution from bone cement? An in vitro comparison between hydrogen peroxide and a mechanical mixer. J. Orthop. Traumatol. Off. J. Ital. Soc. Orthop. Traumatol. 2008, 9, 17–22. [Google Scholar] [CrossRef] [Green Version]
- Rauschmann, M.A.; Wichelhaus, T.A.; Stirnal, V.; Dingeldein, E.; Zichner, L.; Schnettler, R.; Alt, V. Nanocrystalline hydroxyapatite and calcium sulphate as biodegradable composite carrier material for local delivery of antibiotics in bone infections. Biomaterials 2005, 26, 2677–2684. [Google Scholar] [CrossRef]
- Faigle, G.; Bernstein, A.; Suedkamp, N.P.; Mayr, H.O.; Peters, F.; Huebner, W.D.; Seidenstuecker, M. Release behavior of Vancomycin from four types of CaP-Ceramics using various loading methods at two different degrees of acidity. J. Mater. Sci. Mater. Med. 2017, 29. [Google Scholar] [CrossRef]
- Stemberger, A.; Grimm, H.; Bader, F.; Rahn, H.D.; Ascherl, R. Local treatment of bone and soft tissue infections with the collagen–gentamicin sponge. Eur. J. Surg. 1997, 163, 17–26. [Google Scholar]
- Firsov, A.A.; Nazarov, A.D.; Fomina, I.P. Biodegradable implants containing gentamicin: Drug release and pharmacokinetics. Drug Dev. Ind. Pharm. 1987, 13, 1651–1674. [Google Scholar] [CrossRef]
- Friess, W. Collagen–biomaterial for drug delivery. Eur. J. Pharm. Biopharm. 1998, 45, 113–136. [Google Scholar] [CrossRef]
- Scaglione, F. Pharmacotherapy—The facts and fantasies of prophylaxis and combined therapies. Eur. J. Surg 1997, 163, 11–16. [Google Scholar]
- Stemberger, A.; Unkauf, M.; Arnold, D.E.; Blumel, G. Drug carrier systems based on resorbable polyester collagen and/or biomaterial combinations. In Cosmetic and Pharmaceutical Applications of Polymers; Gebelein, C.G., Cheng, T.C., Yang, C.C.-M., Eds.; Plenum Press: New York, NY, USA, 1990; pp. 263–268. [Google Scholar]
- McLaren, A.C.; McLaren, S.G.; McLemore, R.; Vernon, B.L. Particle size of fillers affects permeability of polymethylmethacrylate. Clin. Orthop. Relat. Res. 2007, 461, 64–67. [Google Scholar] [CrossRef]
- Wachol-Drewek, Z.; Pfeiffer, M.; Scholl, E. Comparative investigation of drug delivery of collagen implants saturated in antibiotic solutions and a sponge containing gentamicin. Biomaterials 1996, 17, 1733–1738. [Google Scholar] [CrossRef]









| - | Antibiotics Uptake in wt % | |||
|---|---|---|---|---|
| - | Gentamycin | Vancomycin | ||
| - | Mean | Standard Deviation | Mean | Standard Deviation |
| Osbone® Granulate | 6.50 | 1.18 | 7.48 | 0.86 |
| Cerasorb® M Granulate | 2.65 | 0.56 | 5.15 | 1.00 |
| Cerasorb® Foam | 12.69 | 2.95 | 12.08 | 4.05 |
| - | Gentamycin | Vancomycin | ||||
|---|---|---|---|---|---|---|
| - | Mean Release after 24 h (µg/mL) | Mean Uptake (µg/mL) | Biomaterial Amount to Reach MBEC (mg) | Mean Release after 24 h (µg/mL) | Mean Uptake (µg/mL) | Biomaterial Amount to Reach MBEC (mg) |
| Osbone® Granulate | 512 | 1295 | 494 | 571.6 | 1496 | 214 |
| Cerasorb® M Granulate | 460.8 | 530 | 1208 | 446 | 1032 | 310 |
| Cerasorb® Foam | 1424.2 | 2540 | 252 | 1184 | 2408 | 133 |
| - | Gentamicin | Vancomycin | ||
|---|---|---|---|---|
| - | % after 24 h | Minimum Amount to Reach MBEC (mg) | % after 24 h | Minimum Amount to Reach MBEC (mg) |
| Osbone® Granules | 94.5 | 467 | 96.8 | 207 |
| Cerasorb® M Granules | 99.2 | 1198 | 96.3 | 299 |
| Cerasorb® Foam | 72.3 | 182 | 72 | 96 |
| Material | Condition | Equation |
|---|---|---|
| Cerasorb® Foam | if day ≤ 2.761 | log10(Antibiotics release) = 3.905–0.733 × day |
| Cerasorb® Foam | if day > 2.76 | log10(Antibiotics release) = 2.991–0.402 × day |
| Cerasorb® Granules | if day ≤ 2.76 | log10(Antibiotics release) = 4.524–1.748 × day |
| Cerasorb® Granules | if day > 2.76 | log10(Antibiotics release) = −0.144–0.057 × day |
| Osbone® Granules | if day ≤ 2.76 | log10(Antibiotics release) = 4.349–1.622 × day |
| Osbone® Granules | if day > 2.76 | log10(Antibiotics release) = −0.085–0.016 × day |
| Material | Condition | Equation |
|---|---|---|
| Cerasorb® Foam | if day ≤ 2.76 | log10(Antibiotics release) = 3.407–0.470 × day |
| Cerasorb® Foam | if day > 2.76 | log10(Antibiotics release) = 2.882–0.280 × day |
| Cerasorb® Granules | if day ≤ 2.76 | log10(Antibiotics release) = 3.850–1.353 × day |
| Cerasorb® Granules | if day > 2.76 | log10(Antibiotics release) = 0.124–0.003 × day |
| Osbone® Granules | if day ≤ 2.76 | log10(Antibiotics release) = 4.169–1.468 × day |
| Osbone® Granules | if day > 2.76 | log10(Antibiotics release) = 0.125–0.004 × day |
| - | Gentamicin | Vancomycin | ||
|---|---|---|---|---|
| - | % after 24 h | Minimum Amount to Reach MBEC (mg) | % after 24 h | Minimum Amount to Reach MBEC (mg) |
| Osbone® Granules | 94.5 | 467 | 96.8 | 207 |
| Cerasorb® M Granules | 99.2 | 1198 | 96.3 | 299 |
| Cerasorb® Foam | 72.3 | 182 | 72 | 96 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roth, K.E.; Maier, G.S.; Schmidtmann, I.; Eigner, U.; Hübner, W.D.; Peters, F.; Drees, P.; Maus, U. Release of Antibiotics Out of a Moldable Collagen-β-Tricalciumphosphate-Composite Compared to Two Calcium Phosphate Granules. Materials 2019, 12, 4056. https://doi.org/10.3390/ma12244056
Roth KE, Maier GS, Schmidtmann I, Eigner U, Hübner WD, Peters F, Drees P, Maus U. Release of Antibiotics Out of a Moldable Collagen-β-Tricalciumphosphate-Composite Compared to Two Calcium Phosphate Granules. Materials. 2019; 12(24):4056. https://doi.org/10.3390/ma12244056
Chicago/Turabian StyleRoth, Klaus Edgar, Gerrit Steffen Maier, Irene Schmidtmann, Ulrich Eigner, Wolf Dietrich Hübner, Fabian Peters, Philipp Drees, and Uwe Maus. 2019. "Release of Antibiotics Out of a Moldable Collagen-β-Tricalciumphosphate-Composite Compared to Two Calcium Phosphate Granules" Materials 12, no. 24: 4056. https://doi.org/10.3390/ma12244056
APA StyleRoth, K. E., Maier, G. S., Schmidtmann, I., Eigner, U., Hübner, W. D., Peters, F., Drees, P., & Maus, U. (2019). Release of Antibiotics Out of a Moldable Collagen-β-Tricalciumphosphate-Composite Compared to Two Calcium Phosphate Granules. Materials, 12(24), 4056. https://doi.org/10.3390/ma12244056