Combined Proteomics/Genomics Approach Reveals Proteomic Changes of Mature Virions as a Novel Poxvirus Adaptation Mechanism
Abstract
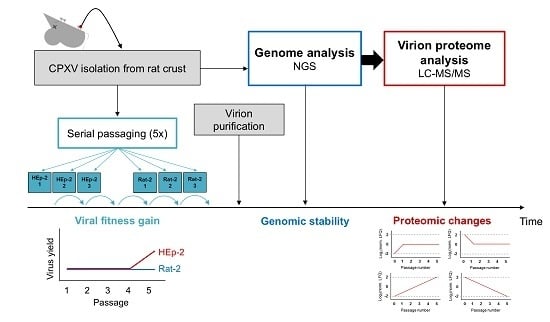
:1. Introduction
2. Materials and Methods
2.1. Virus Isolation from Rat Crust
2.2. Mature Virion Purification
2.3. Serial Passaging
2.4. Plaque Assay and Determination of Genome Equivalents
2.5. Determination of the GE-to-PFU Ratio in the Supernatant
2.6. Real-Time Cell Analysis
2.7. Next-Generation Sequencing (NGS)
2.8. NGS Data Analysis
2.9. Sample Preparation for LC-MS/MS
2.10. LC-MS/MS Analysis
2.11. Proteomic Data Analysis
3. Results
3.1. Replication Gain during Passaging in Human Cells
3.2. Real-Time Cell Analysis Indicates Heterogeneities of the Crust Isolate
3.3. Genome Analysis of CPXV Crust and Passages
Variant Analysis Reveals Only Minor Variants during Passaging
3.4. Proteome Analysis of CPXV Crust and Passages
3.4.1. Changes of Viral Proteins during Passaging
3.4.2. Changes of Host Proteins during Passaging
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Hematian, A.; Sadeghifard, N.; Mohebi, R.; Taherikalani, M.; Nasrolahi, A.; Amraei, M.; Ghafourian, S. Traditional and modern cell culture in virus diagnosis. Osong Public Health Res. Perspect. 2016, 7, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Koprowski, H.; Lennette, E.H. Effect of in vitro cultivation on the pathogenicity of West Nile virus. J. Bacteriol. 1946, 51, 617. [Google Scholar] [CrossRef] [PubMed]
- Randall, C.C.; Ryden, F.W. Adaptation of vaccinia virus to Earle’s L-cells with prolonged noninfectious period. Proc. Soc. Exp. Biol. Med. 1960, 103, 723–725. [Google Scholar] [CrossRef] [PubMed]
- Lundkvist, A.; Cheng, Y.; Sjolander, K.B.; Niklasson, B.; Vaheri, A.; Plyusnin, A. Cell culture adaptation of puumala hantavirus changes the infectivity for its natural reservoir, Clethrionomys glareolus and leads to accumulation of mutants with altered genomic RNA s segment. J. Virol. 1997, 71, 9515–9523. [Google Scholar] [PubMed]
- Bankamp, B.; Fontana, J.M.; Bellini, W.J.; Rota, P.A. Adaptation to cell culture induces functional differences in measles virus proteins. Virol. J. 2008, 5, 129. [Google Scholar] [CrossRef] [PubMed]
- Mohapatra, J.K.; Pandey, L.K.; Rai, D.K.; Das, B.; Rodriguez, L.L.; Rout, M.; Subramaniam, S.; Sanyal, A.; Rieder, E.; Pattnaik, B. Cell culture adaptation mutations in foot-and-mouth disease virus serotype a capsid proteins: Implications for receptor interactions. J. Gen. Virol. 2015, 96, 553–564. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.D.; Lee, G.C.; Kim, Y.Y.; Lee, C.H. A comparison between low- and high-passage strains of human cytomegalovirus. J. Microbiol. Biotechnol. 2016, 26, 1800–1807. [Google Scholar] [CrossRef] [PubMed]
- Sanjuan, R.; Nebot, M.R.; Chirico, N.; Mansky, L.M.; Belshaw, R. Viral mutation rates. J. Virol. 2010, 84, 9733–9748. [Google Scholar] [CrossRef] [PubMed]
- Aubertin, A.M.; McAuslan, B.R. Virus-associated nucleases: Evidence for endonuclease and exonuclease activity in rabbitpox and vaccinia viruses. J. Virol. 1972, 9, 554–556. [Google Scholar] [PubMed]
- Caradonna, S.; Worrad, D.; Lirette, R. Isolation of a herpes simplex virus cDNA encoding the DNA repair enzyme uracil-DNA glycosylase. J. Virol. 1987, 61, 3040–3047. [Google Scholar] [PubMed]
- Moss, B. Poxvirus DNA replication. Cold Spring Harb. Perspect. Biol. 2013, 5. [Google Scholar] [CrossRef] [PubMed]
- Qin, L.; Evans, D.H. Genome scale patterns of recombination between coinfecting vaccinia viruses. J. Virol. 2014, 88, 5277–5286. [Google Scholar] [CrossRef] [PubMed]
- Culyba, M.J.; Minkah, N.; Hwang, Y.; Benhamou, O.M.; Bushman, F.D. DNA branch nuclease activity of vaccinia A22 resolvase. J. Biol. Chem. 2007, 282, 34644–34652. [Google Scholar] [CrossRef] [PubMed]
- Eckert, D.; Williams, O.; Meseda, C.A.; Merchlinsky, M. Vaccinia virus nicking-joining enzyme is encoded by K4L (vacwr035). J. Virol. 2005, 79, 15084–15090. [Google Scholar] [CrossRef] [PubMed]
- Stuart, D.T.; Upton, C.; Higman, M.A.; Niles, E.G.; McFadden, G. A poxvirus-encoded uracil DNA glycosylase is essential for virus viability. J. Virol. 1993, 67, 2503–2512. [Google Scholar] [PubMed]
- Werden, S.J.; Rahman, M.M.; McFadden, G. Poxvirus host range genes. Adv. Virus Res. 2008, 71, 135–171. [Google Scholar] [CrossRef] [PubMed]
- Lewis-Jones, S. Zoonotic poxvirus infections in humans. Curr. Opin. Infect. Dis. 2004, 17, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Vorou, R.M.; Papavassiliou, V.G.; Pierroutsakos, I.N. Cowpox virus infection: An emerging health threat. Curr. Opin. Infect. Dis. 2008, 21, 153–156. [Google Scholar] [CrossRef] [PubMed]
- Shchelkunov, S.N. An increasing danger of zoonotic orthopoxvirus infections. PLoS Pathog. 2013, 9, e1003756. [Google Scholar] [CrossRef] [PubMed]
- Elde, N.C.; Child, S.J.; Eickbush, M.T.; Kitzman, J.O.; Rogers, K.S.; Shendure, J.; Geballe, A.P.; Malik, H.S. Poxviruses deploy genomic accordions to adapt rapidly against host antiviral defenses. Cell 2012, 150, 831–841. [Google Scholar] [CrossRef] [PubMed]
- Cone, K.R.; Kronenberg, Z.N.; Yandell, M.; Elde, N.C. Emergence of a viral RNA polymerase variant during gene copy number amplification promotes rapid evolution of vaccinia virus. J. Virol. 2017, 91. [Google Scholar] [CrossRef] [PubMed]
- Brennan, G.; Kitzman, J.O.; Shendure, J.; Geballe, A.P. Experimental evolution identifies vaccinia virus mutations in A24R and A35R that antagonize the protein kinase R pathway and accompany collapse of an extragenic gene amplification. J. Virol. 2015, 89, 9986–9997. [Google Scholar] [CrossRef] [PubMed]
- Hendrickson, R.C.; Wang, C.; Hatcher, E.L.; Lefkowitz, E.J. Orthopoxvirus genome evolution: The role of gene loss. Viruses 2010, 2, 1933–1967. [Google Scholar] [CrossRef] [PubMed]
- Dumbell, K.R.; Bedson, H.S. The use of ceiling temperature and reactivation in the isolation of pox virus hybrids. J. Hyg. 1964, 62, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Cresawn, S.G.; Prins, C.; Latner, D.R.; Condit, R.C. Mapping and phenotypic analysis of spontaneous isatin-β-thiosemicarbazone resistant mutants of vaccinia virus. Virology 2007, 363, 319–332. [Google Scholar] [CrossRef] [PubMed]
- Condit, R.C.; Easterly, R.; Pacha, R.F.; Fathi, Z.; Meis, R.J. A vaccinia virus isatin-β-thiosemicarbazone resistance mutation maps in the viral gene encoding the 132-kDa subunit of RNA polymerase. Virology 1991, 185, 857–861. [Google Scholar] [CrossRef]
- Prins, C.; Cresawn, S.G.; Condit, R.C. An isatin-β-thiosemicarbazone-resistant vaccinia virus containing a mutation in the second largest subunit of the viral RNA polymerase is defective in transcription elongation. J. Biol. Chem. 2004, 279, 44858–44871. [Google Scholar] [CrossRef] [PubMed]
- Condit, R.C.; Niles, E.G. Regulation of viral transcription elongation and termination during vaccinia virus infection. Biochim. Biophys. Acta 2002, 1577, 325–336. [Google Scholar] [CrossRef]
- Earl, P.L.; Moss, B.; Wyatt, L.S.; Carroll, M.W. Generation of recombinant vaccinia viruses. Curr. Protoc. Mol. Biol. 2001. [Google Scholar] [CrossRef]
- Doellinger, J.; Schaade, L.; Nitsche, A. Comparison of the cowpox virus and vaccinia virus mature virion proteome: Analysis of the species- and strain-specific proteome. PLoS ONE 2015, 10, e0141527. [Google Scholar] [CrossRef] [PubMed]
- Witkowski, P.T.; Schuenadel, L.; Wiethaus, J.; Bourquain, D.R.; Kurth, A.; Nitsche, A. Cellular impedance measurement as a new tool for poxvirus titration, antibody neutralization testing and evaluation of antiviral substances. Biochem. Biophys. Res. Commun. 2010, 401, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Bolger, A.M.; Lohse, M.; Usadel, B. Trimmomatic: A flexible trimmer for Illumina sequence data. Bioinformatics 2014, 30, 2114–2120. [Google Scholar] [CrossRef] [PubMed]
- FastQC. Available online: http://www.bioinformatics.babraham.ac.uk/projects/fastqc/ (accessed on 16 August 2017).
- Tausch, S.H.; Renard, B.Y.; Nitsche, A.; Dabrowski, P.W. RAMBO-K: Rapid and sensitive removal of background sequences from next generation sequencing data. PLoS ONE 2015, 10, e0137896. [Google Scholar] [CrossRef] [PubMed]
- Bankevich, A.; Nurk, S.; Antipov, D.; Gurevich, A.A.; Dvorkin, M.; Kulikov, A.S.; Lesin, V.M.; Nikolenko, S.I.; Pham, S.; Prjibelski, A.D.; et al. Spades: A new genome assembly algorithm and its applications to single-cell sequencing. J. Comput. Biol. 2012, 19, 455–477. [Google Scholar] [CrossRef] [PubMed]
- Zerbino, D.R.; Birney, E. Velvet: Algorithms for de novo short read assembly using de Bruijn graphs. Genome Res. 2008, 18, 821–829. [Google Scholar] [CrossRef] [PubMed]
- Langmead, B.; Salzberg, S.L. Fast gapped-read alignment with Bowtie 2. Nat. Methods 2012, 9, 357–359. [Google Scholar] [CrossRef] [PubMed]
- Kearse, M.; Moir, R.; Wilson, A.; Stones-Havas, S.; Cheung, M.; Sturrock, S.; Buxton, S.; Cooper, A.; Markowitz, S.; Duran, C.; et al. Geneious basic: An integrated and extendable desktop software platform for the organization and analysis of sequence data. Bioinformatics 2012, 28, 1647–1649. [Google Scholar] [CrossRef] [PubMed]
- Wisniewski, J.R.; Zougman, A.; Nagaraj, N.; Mann, M. Universal sample preparation method for proteome analysis. Nat. Methods 2009, 6, 359–362. [Google Scholar] [CrossRef] [PubMed]
- Ishihama, Y.; Rappsilber, J.; Mann, M. Modular stop and go extraction tips with stacked disks for parallel and multidimensional peptide fractionation in proteomics. J. Proteome Res. 2006, 5, 988–994. [Google Scholar] [CrossRef] [PubMed]
- Vizcaino, J.A.; Csordas, A.; del-Toro, N.; Dianes, J.A.; Griss, J.; Lavidas, I.; Mayer, G.; Perez-Riverol, Y.; Reisinger, F.; Ternent, T.; et al. 2016 update of the PRIDE database and its related tools. Nucleic Acids Res. 2016, 44, 11033. [Google Scholar] [CrossRef] [PubMed]
- Bielow, C.; Mastrobuoni, G.; Kempa, S. Proteomics quality control: Quality control software for MaxQuant results. J. Proteome Res. 2016, 15, 777–787. [Google Scholar] [CrossRef] [PubMed]
- Steinhardt, E.; Israeli, C.; Lambert, R.A. Studies on the cultivation of the virus of vaccinia. J. Infect. Dis. 1913, 13, 294–300. [Google Scholar] [CrossRef]
- Sharp, D.G.; Sadhukhan, P.; Galasso, G.J. Quality changes in vaccinia virus during adaptation to growth in cultures of Earle’s L cells. J. Bacteriol. 1964, 88, 309–312. [Google Scholar] [PubMed]
- Vanderplasschen, A.; Mathew, E.; Hollinshead, M.; Sim, R.B.; Smith, G.L. Extracellular enveloped vaccinia virus is resistant to complement because of incorporation of host complement control proteins into its envelope. Proc. Natl. Acad. Sci. USA 1998, 95, 7544–7549. [Google Scholar] [CrossRef] [PubMed]
- Meyer, H.; Sutter, G.; Mayr, A. Mapping of deletions in the genome of the highly attenuated vaccinia virus MVA and their influence on virulence. J. Gen. Virol. 1991, 72 Pt 5, 1031–1038. [Google Scholar] [CrossRef] [PubMed]
- Hatcher, E.L.; Wang, C.; Lefkowitz, E.J. Genome variability and gene content in chordopoxviruses: Dependence on microsatellites. Viruses 2015, 7, 2126–2146. [Google Scholar] [CrossRef] [PubMed]
- Knutson, B.A.; Broyles, S.S. Expansion of poxvirus RNA polymerase subunits sharing homology with corresponding subunits of RNA polymerase II. Virus Genes 2008, 36, 307–311. [Google Scholar] [CrossRef] [PubMed]
- Moss, B.; Ahn, B.Y.; Amegadzie, B.; Gershon, P.D.; Keck, J.G. Cytoplasmic transcription system encoded by vaccinia virus. J. Biol. Chem. 1991, 266, 1355–1358. [Google Scholar] [PubMed]
- Patel, D.D.; Pickup, D.J. The second-largest subunit of the poxvirus RNA polymerase is similar to the corresponding subunits of procaryotic and eucaryotic RNA polymerases. J. Virol. 1989, 63, 1076–1086. [Google Scholar] [PubMed]
- Davies, M.V.; Elroy-Stein, O.; Jagus, R.; Moss, B.; Kaufman, R.J. The vaccinia virus K3l gene product potentiates translation by inhibiting double-stranded-RNA-activated protein kinase and phosphorylation of the α subunit of eukaryotic initiation factor 2. J. Virol. 1992, 66, 1943–1950. [Google Scholar] [PubMed]
- Davies, M.V.; Chang, H.W.; Jacobs, B.L.; Kaufman, R.J. The E3l and K3l vaccinia virus gene products stimulate translation through inhibition of the double-stranded RNA-dependent protein kinase by different mechanisms. J. Virol. 1993, 67, 1688–1692. [Google Scholar] [PubMed]
- Latner, D.R.; Xiang, Y.; Lewis, J.I.; Condit, J.; Condit, R.C. The vaccinia virus bifunctional gene J3 (nucleoside-2′-O-)-methyltransferase and poly(A) polymerase stimulatory factor is implicated as a positive transcription elongation factor by two genetic approaches. Virology 2000, 269, 345–355. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.J.; Chang, Y.X.; Izmailyan, R.; Tang, Y.L.; Chang, W. Vaccinia virus A25 and A26 proteins are fusion suppressors for mature virions and determine strain-specific virus entry pathways into HeLa, CHO-K1 and L cells. J. Virol. 2010, 84, 8422–8432. [Google Scholar] [CrossRef] [PubMed]
- Bengali, Z.; Satheshkumar, P.S.; Moss, B. Orthopoxvirus species and strain differences in cell entry. Virology 2012, 433, 506–512. [Google Scholar] [CrossRef] [PubMed]
- Bengali, Z.; Townsley, A.C.; Moss, B. Vaccinia virus strain differences in cell attachment and entry. Virology 2009, 389, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Husain, M.; Moss, B. Vaccinia virus F13L protein with a conserved phospholipase catalytic motif induces colocalization of the B5R envelope glycoprotein in post-Golgi vesicles. J. Virol. 2001, 75, 7528–7542. [Google Scholar] [CrossRef] [PubMed]
- Bidgood, S.R.; Mercer, J. Cloak and dagger: Alternative immune evasion and modulation strategies of poxviruses. Viruses 2015, 7, 4800–4825. [Google Scholar] [CrossRef] [PubMed]
- Vliegen, I.; Yang, G.; Hruby, D.; Jordan, R.; Neyts, J. Deletion of the vaccinia virus F13L gene results in a highly attenuated virus that mounts a protective immune response against subsequent vaccinia virus challenge. Antivir. Res. 2012, 93, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Doceul, V.; Hollinshead, M.; Breiman, A.; Laval, K.; Smith, G.L. Protein B5 is required on extracellular enveloped vaccinia virus for repulsion of superinfecting virions. J. Gen. Virol. 2012, 93, 1876–1886. [Google Scholar] [CrossRef] [PubMed]
- Doceul, V.; Hollinshead, M.; van der Linden, L.; Smith, G.L. Repulsion of superinfecting virions: A mechanism for rapid virus spread. Science 2010, 327, 873–876. [Google Scholar] [CrossRef] [PubMed]
- Van den Broek, M.F.; Muller, U.; Huang, S.; Zinkernagel, R.M.; Aguet, M. Immune defence in mice lacking type I and/or type II interferon receptors. Immunol. Rev. 1995, 148, 5–18. [Google Scholar] [CrossRef] [PubMed]
- Reading, P.C.; Symons, J.A.; Smith, G.L. A soluble chemokine-binding protein from vaccinia virus reduces virus virulence and the inflammatory response to infection. J. Immunol. 2003, 170, 1435–1442. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, N.; Symons, J.A.; Tscharke, D.C.; Smith, G.L. The vaccinia virus N1L protein is an intracellular homodimer that promotes virulence. J. Gen. Virol. 2002, 83, 1965–1976. [Google Scholar] [CrossRef] [PubMed]
- Isaacs, S.N.; Kotwal, G.J.; Moss, B. Vaccinia virus complement-control protein prevents antibody-dependent complement-enhanced neutralization of infectivity and contributes to virulence. Proc. Natl. Acad. Sci. USA 1992, 89, 628–632. [Google Scholar] [CrossRef] [PubMed]
- Symons, J.A.; Alcami, A.; Smith, G.L. Vaccinia virus encodes a soluble type I interferon receptor of novel structure and broad species specificity. Cell 1995, 81, 551–560. [Google Scholar] [CrossRef]
- Waibler, Z.; Anzaghe, M.; Frenz, T.; Schwantes, A.; Pohlmann, C.; Ludwig, H.; Palomo-Otero, M.; Alcami, A.; Sutter, G.; Kalinke, U. Vaccinia virus-mediated inhibition of type I interferon responses is a multifactorial process involving the soluble type I interferon receptor B18 and intracellular components. J. Virol. 2009, 83, 1563–1571. [Google Scholar] [CrossRef] [PubMed]
- Alcami, A.; Symons, J.A.; Smith, G.L. The vaccinia virus soluble α/β interferon (IFN) receptor binds to the cell surface and protects cells from the antiviral effects of IFN. J. Virol. 2000, 74, 11230–11239. [Google Scholar] [CrossRef] [PubMed]
- Girgis, N.M.; Dehaven, B.C.; Xiao, Y.; Alexander, E.; Viner, K.M.; Isaacs, S.N. The vaccinia virus complement control protein modulates adaptive immune responses during infection. J. Virol. 2011, 85, 2547–2556. [Google Scholar] [CrossRef] [PubMed]
- Alcami, A.; Symons, J.A.; Collins, P.D.; Williams, T.J.; Smith, G.L. Blockade of chemokine activity by a soluble chemokine binding protein from vaccinia virus. J. Immunol. 1998, 160, 624–633. [Google Scholar] [PubMed]
- DiPerna, G.; Stack, J.; Bowie, A.G.; Boyd, A.; Kotwal, G.; Zhang, Z.; Arvikar, S.; Latz, E.; Fitzgerald, K.A.; Marshall, W.L. Poxvirus protein N1L targets the I-κB kinase complex, inhibits signaling to NF-κB by the tumor necrosis factor superfamily of receptors and inhibits NF-κB and IRF3 signaling by toll-like receptors. J. Biol. Chem. 2004, 279, 36570–36578. [Google Scholar] [CrossRef] [PubMed]
- Maluquer de Motes, C.; Schiffner, T.; Sumner, R.P.; Smith, G.L. Vaccinia virus virulence factor N1 can be ubiquitylated on multiple lysine residues. J. Gen. Virol. 2014, 95, 2038–2049. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Abrahams, M.R.; Hunt, L.A.; Suttles, J.; Marshall, W.; Lahiri, D.K.; Kotwal, G.J. The vaccinia virus N1L protein influences cytokine secretion in vitro after infection. Ann. N. Y. Acad. Sci. 2005, 1056, 69–86. [Google Scholar] [CrossRef] [PubMed]
- Almazan, F.; Tscharke, D.C.; Smith, G.L. The vaccinia virus superoxide dismutase-like protein (A45R) is a virion component that is nonessential for virus replication. J. Virol. 2001, 75, 7018–7029. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.C.; Li, J.; Irwin, C.R.; Jenkins, H.; DeLange, L.; Evans, D.H. Vaccinia virus DNA ligase recruits cellular topoisomerase II to sites of viral replication and assembly. J. Virol. 2008, 82, 5922–5932. [Google Scholar] [CrossRef] [PubMed]
- Prichard, M.N.; Kern, E.R.; Quenelle, D.C.; Keith, K.A.; Moyer, R.W.; Turner, P.C. Vaccinia virus lacking the deoxyuridine triphosphatase gene (F2L) replicates well in vitro and in vivo but is hypersensitive to the antiviral drug (N)-methanocarbathymidine. Virol. J. 2008, 5, 39. [Google Scholar] [CrossRef] [PubMed]
- Senkevich, T.G.; White, C.L.; Koonin, E.V.; Moss, B. Complete pathway for protein disulfide bond formation encoded by poxviruses. Proc. Natl. Acad. Sci. USA 2002, 99, 6667–6672. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, F.I.; Bleck, C.K.; Reh, L.; Novy, K.; Wollscheid, B.; Helenius, A.; Stahlberg, H.; Mercer, J. Vaccinia virus entry is followed by core activation and proteasome-mediated release of the immunomodulatory effector VH1 from lateral bodies. Cell. Rep. 2013, 4, 464–476. [Google Scholar] [CrossRef] [PubMed]
- White, C.L.; Senkevich, T.G.; Moss, B. Vaccinia virus G4L glutaredoxin is an essential intermediate of a cytoplasmic disulfide bond pathway required for virion assembly. J. Virol. 2002, 76, 467–472. [Google Scholar] [CrossRef] [PubMed]
- White, C.L.; Weisberg, A.S.; Moss, B. A glutaredoxin, encoded by the G4L gene of vaccinia virus, is essential for virion morphogenesis. J. Virol. 2000, 74, 9175–9183. [Google Scholar] [CrossRef] [PubMed]
- Pauli, G.; Blumel, J.; Burger, R.; Drosten, C.; Groner, A.; Gurtler, L.; Heiden, M.; Hildebrandt, M.; Jansen, B.; Montag-Lessing, T.; et al. Orthopox viruses: Infections in humans. Transfus. Med. Hemother. 2010, 37, 351–364. [Google Scholar] [CrossRef] [PubMed]
- Krauss, O.; Hollinshead, R.; Hollinshead, M.; Smith, G.L. An investigation of incorporation of cellular antigens into vaccinia virus particles. J. Gen. Virol. 2002, 83, 2347–2359. [Google Scholar] [CrossRef] [PubMed]
- Castro, A.P.; Carvalho, T.M.; Moussatche, N.; Damaso, C.R. Redistribution of cyclophilin A to viral factories during vaccinia virus infection and its incorporation into mature particles. J. Virol. 2003, 77, 9052–9068. [Google Scholar] [CrossRef] [PubMed]
- Boone, R.F.; Moss, B. Sequence complexity and relative abundance of vaccinia virus mRNA’s synthesized in vivo and in vitro. J. Virol. 1978, 26, 554–569. [Google Scholar] [PubMed]
- Liem, J.; Liu, J. Stress beyond translation: Poxviruses and more. Viruses 2016, 8, 169. [Google Scholar] [CrossRef] [PubMed]
- Nerenberg, B.T.; Taylor, J.; Bartee, E.; Gouveia, K.; Barry, M.; Fruh, K. The poxviral RING protein p28 is a ubiquitin ligase that targets ubiquitin to viral replication factories. J. Virol. 2005, 79, 597–601. [Google Scholar] [CrossRef] [PubMed]
- Katsafanas, G.C.; Moss, B. Vaccinia virus intermediate stage transcription is complemented by Ras-GTPase-activating protein SH3 domain-binding protein (G3BP) and cytoplasmic activation/proliferation-associated protein (p137) individually or as a heterodimer. J. Biol. Chem. 2004, 279, 52210–52217. [Google Scholar] [CrossRef] [PubMed]
- Dellis, S.; Strickland, K.C.; McCrary, W.J.; Patel, A.; Stocum, E.; Wright, C.F. Protein interactions among the vaccinia virus late transcription factors. Virology 2004, 329, 328–336. [Google Scholar] [CrossRef] [PubMed]
- Wright, C.F.; Oswald, B.W.; Dellis, S. Vaccinia virus late transcription is activated in vitro by cellular heterogeneous nuclear ribonucleoproteins. J. Biol. Chem. 2001, 276, 40680–40686. [Google Scholar] [CrossRef] [PubMed]
- Machesky, L.M.; Cole, N.B.; Moss, B.; Pollard, T.D. Vaccinia virus expresses a novel profilin with a higher affinity for polyphosphoinositides than actin. Biochemistry 1994, 33, 10815–10824. [Google Scholar] [CrossRef] [PubMed]
- Husain, M.; Moss, B. Similarities in the induction of post-Golgi vesicles by the vaccinia virus F13L protein and phospholipase D. J. Virol. 2002, 76, 7777–7789. [Google Scholar] [CrossRef] [PubMed]
- Peters, N.E.; Ferguson, B.J.; Mazzon, M.; Fahy, A.S.; Krysztofinska, E.; Arribas-Bosacoma, R.; Pearl, L.H.; Ren, H.; Smith, G.L. A mechanism for the inhibition of DNA-PK-mediated DNA sensing by a virus. PLoS Pathog. 2013, 9, e1003649. [Google Scholar] [CrossRef] [PubMed]
- Tran, K.; Mahr, J.A.; Spector, D.H. Proteasome subunits relocalize during human cytomegalovirus infection and proteasome activity is necessary for efficient viral gene transcription. J. Virol. 2010, 84, 3079–3093. [Google Scholar] [CrossRef] [PubMed]




| CDS a | Pos. b | Nucleotide Change | PE c | Amino Acid Change | Variant Frequency HEp-2 | Variant Frequency Rat-2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P0 | P1 | P2 | P3 | P4 | P5 | P1 | P2 | P3 | P4 | P5 | |||||
| A12R | 728 | A→G | S | K→R | 1.2 | ||||||||||
| A24R | 1149 | (A)8→(A)9 | FS | none | 1.4 | ||||||||||
| A25R | 269 | A→C | S | K→T | 3.1 | 2.7 | 4.2 | 6.4 | 2.9 | 11.4 | 2.2 | 4.2 | 2.7 | 9.5 | 4.6 |
| A25R | 4 | (A)8→(A)9 | FS | 1.3 | 1.4 | ||||||||||
| A26L | 1091 | G→T | S | H→Q | 1.1 | ||||||||||
| A26L | 1118 | (GTT)8→(GTT)9 | I | P→QP | 3.1 | 2.7 | 2.9 | 2.6 | 3.4 | 2.6 | 4.2 | 2.5 | |||
| A26L | 1115 | (GTT)8→(GTT)7 | D | QP→P | 4.6 | 4.3 | 3.8 | 3.8 | 4.2 | 4.6 | |||||
| A26L | 1093 | (TTG)8→(TTG)7 | D | Q→ | 3.7 | 5.0 | 3.4 | ||||||||
| A26L | 1093 | (TTG)8→(TTG)9 | I | →Q | 4.0 | 2.6 | 2.8 | ||||||||
| A9R | 259 | (A)8→(A)9 | FS | 1.5 | |||||||||||
| C1L | 465 | C→A | S | R→S | 1.2 | ||||||||||
| C2L | 168 | C→T | N | none | 1.5 | ||||||||||
| D6L | 613 | ATA→TCC | S | Y→G | 1.9 | ||||||||||
| D6L | 615 | A→T | T | 1.0 | 1.1 | ||||||||||
| D6L | 616 | +TCC | I | →G | 8.8 | 7.4 | |||||||||
| D6L | 611 | C→T | S | S→N | 8.7 | 7.4 | |||||||||
| D6L | 606 | G→A | N | none | 8.5 | 7.1 | |||||||||
| E10R | 474 | (T)7→(T)8 | FS | 2.9 | 2.0 | 1.7 | 2.2 | ||||||||
| E10R | 481 | (T)7→(T)8 | FS | 2.6 | |||||||||||
| E10R | 716 | A→T | S | E→V | 1.8 | ||||||||||
| H3R | 28 | A→G | S | N→D | 1.3 | ||||||||||
| J4L | 101 | +GG | FS | 1.1 | |||||||||||
| J6R | 319 | A→G | S | K→E | 2.1 | ||||||||||
| L6L | 1084 | (T)10→(T)11 | FS | 1.9 | |||||||||||
| O4R | 1648 | T→C | S | S→P | 1.1 | ||||||||||
| Protein | Description a | Function |
|---|---|---|
| HEp-2 | ||
| A34 | EEV glycoprotein | membrane |
| E8 | Cell-surface-binding protein | membrane |
| E13 | Scaffold protein | membrane |
| B17 | Soluble IFN-α/β receptor | immune evasion |
| C17 | Complement control protein | immune evasion |
| D1/I5 | Secreted chemokine-binding protein | immune evasion |
| Q1 | Inhibitor of TNF-R and TLR signaling | immune evasion |
| C6 | Uncharacterized protein | unknown |
| C10 | Uncharacterized protein | unknown |
| F2 | Uncharacterized protein | unknown |
| G16 | Uncharacterized protein | unknown |
| A48 | Cu-Zn superoxide dismutase-like protein | others |
| G2 | dUTPase | others |
| H4 | Glutaredoxin-2 | others |
| A53 | DNA ligase | DNA replication |
| Rat-2 | ||
| B4 | EEV type-I membrane glycoprotein | membrane |
| A50 | Uncharacterized protein | unknown |
| A52 | Uncharacterized protein | unknown |
| B3 | Uncharacterized protein | unknown |
| C14 | Uncharacterized protein | unknown |
| B7 | IFN-γ receptor-like protein | immune evasion |
| Q1 | Inhibitor of TNF-R and TLR signaling | immune evasion |
| A53 | DNA ligase | DNA replication |
| Gene name | Description | Enrichment in OPV IMV a | Enrichment during Passaging b | ||||
|---|---|---|---|---|---|---|---|
| P1 | P2 | P3 | P4 | P5 | |||
| HEp-2 | |||||||
| PFN-1 | Profilin-1 | 35.1 | 1.3 | 0.5 | −0.1 | −0.6 | −1.1 |
| PGK1 | Phosphoglycerate kinase 1 | 12.9 | 1.2 | 0.6 | 0.2 | −1.3 | −0.6 |
| ARF1 | ADP-ribosylation factor 1 | 12.8 | 1.4 | 0.4 | −0.1 | −1.0 | −0.7 |
| PDCD6 | Programmed cell death protein 6 | 7.2 | 1.3 | 0.6 | −0.5 | −0.9 | −0.6 |
| XRCC5 | X-ray repair cross-complementing protein 5 | 6.6 | −1.1 | −0.6 | −0.2 | 0.5 | 1.4 |
| PRDX6 | Peroxiredoxin-6 | 4.3 | 1.5 | 0.4 | −0.1 | −1.0 | −0.8 |
| ATIC | Bifunctional purine biosynthesis protein | 3.7 | −1.2 | 0.1 | −0.8 | 0.9 | 0.9 |
| ACP1 | Acid phosphatase 1 | 3.3 | 1.2 | 0.6 | 0.1 | −1.1 | −0.8 |
| HSPA8 | Heat shock cognate 71 kDa protein | 2.4 | 1.0 | 0.5 | 0.6 | −1.3 | −0.7 |
| CAD | CAD protein | 2.4 | −1.8 | 0.3 | 0.4 | 0.4 | 0.7 |
| EIF3B | Eukaryotic translation initiation factor 3 subunit | 2.1 | −1.1 | −0.8 | 0.2 | 0.3 | 1.4 |
| MPG | DNA-3-methyladenine glycosylase | 2.0 | 1.2 | 0.5 | 0.0 | −1.2 | −0.6 |
| Rat-2 | |||||||
| Sqstm1 | Sequestosome-1 | 8.3 | 0.5 | 1.2 | 0.0 | −0.5 | −1.2 |
| Dstn | Destrin | 7.6 | 1.1 | −0.2 | 0.5 | 0.0 | −1.4 |
| Itpa | Inosine triphosphate pyrophosphatase | 4.6 | −1.4 | −0.2 | 0.5 | 0.7 | 0.5 |
| Phb2 | Prohibitin-2 | 3.4 | 1.0 | 0.9 | −0.6 | −0.3 | −1.0 |
| Psmc5 | 26S protease regulatory subunit 8 | 3.4 | −1.1 | −0.8 | 0.4 | 0.7 | 0.9 |
| Eif3b | Eukaryotic translation initiation factor 3 subunit B | 2.1 | −0.9 | −1.0 | 0.3 | 0.8 | 0.8 |
| Dnajc7 | DnaJ homolog subfamily C member 7 | 2.1 | 0.8 | 0.6 | −0.1 | 0.3 | −1.6 |
| Rab6a | Ras-related protein Rab-6A | 2.0 | 0.5 | 1.2 | −0.3 | −0.3 | −1.2 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grossegesse, M.; Doellinger, J.; Tyshaieva, A.; Schaade, L.; Nitsche, A. Combined Proteomics/Genomics Approach Reveals Proteomic Changes of Mature Virions as a Novel Poxvirus Adaptation Mechanism. Viruses 2017, 9, 337. https://doi.org/10.3390/v9110337
Grossegesse M, Doellinger J, Tyshaieva A, Schaade L, Nitsche A. Combined Proteomics/Genomics Approach Reveals Proteomic Changes of Mature Virions as a Novel Poxvirus Adaptation Mechanism. Viruses. 2017; 9(11):337. https://doi.org/10.3390/v9110337
Chicago/Turabian StyleGrossegesse, Marica, Joerg Doellinger, Alona Tyshaieva, Lars Schaade, and Andreas Nitsche. 2017. "Combined Proteomics/Genomics Approach Reveals Proteomic Changes of Mature Virions as a Novel Poxvirus Adaptation Mechanism" Viruses 9, no. 11: 337. https://doi.org/10.3390/v9110337
APA StyleGrossegesse, M., Doellinger, J., Tyshaieva, A., Schaade, L., & Nitsche, A. (2017). Combined Proteomics/Genomics Approach Reveals Proteomic Changes of Mature Virions as a Novel Poxvirus Adaptation Mechanism. Viruses, 9(11), 337. https://doi.org/10.3390/v9110337