Adherence to the Mediterranean Diet in a Portuguese Immigrant Community in the Central Valley of California
Abstract
:1. Introduction
2. Materials and Methods
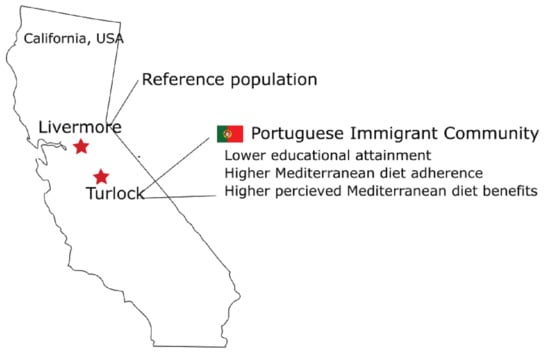
2.1. Study Setting
2.2. Survey Instrument
2.3. Survey Distribution
2.4. Statistical Analyses
3. Results
3.1. Demographic Assessment
3.2. Mediterranean Diet Adherence
3.3. Barriers to Consuming a MedDiet in Turlock
3.4. Benefits to Consuming a MedDiet in Turlock
3.5. Stages of Change and Demographic Influences
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ruthsatz, M.; Candeias, V. Non-communicable disease prevention, nutrition and aging. Acta Biomed. 2020, 91, 379–388. [Google Scholar]
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean diet and multiple health outcomes: An umbrella review of meta-analyses of observational studies and randomised trials. Eur. J. Clin. Nutr. 2018, 72, 30–43. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Galiot, A.; Goñi, I. Adherence to the Mediterranean diet pattern, cognitive status and depressive symptoms in an elderly non-institutionalized population. Nutr. Hosp. 2017, 34, 338–344. [Google Scholar] [CrossRef]
- Kennedy, B.K.; Berger, S.L.; Brunet, A.; Campisi, J.; Cuervo, A.M.; Epel, E.S.; Franceschi, C.; Lithgow, G.J.; Morimoto, R.I.; Pessin, J.E.; et al. Geroscience: Linking aging to chronic disease. Cell 2014, 159, 709–713. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmad, S.; Moorthy, M.V.; Demler, O.V.; Hu, F.B.; Ridker, P.M.; Chasman, D.I.; Mora, S. Assessment of risk factors and biomarkers associated with risk of cardiovascular disease among women consuming a Mediterranean diet. JAMA Netw. Open 2018, 1, e185708. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martinez-Lacoba, R.; Pardo-Garcia, I.; Amo-Saus, E.; Escribano-Sotos, F. Mediterranean diet and health outcomes: A systematic meta-review. Eur. J. Public Health 2018, 28, 955–961. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sánchez-Taínta, A.; Estruch, R.; Bullo, M.; Corella, D.; Gomez-Gracia, E.; Fiol, M.; Algorta, J.; Covas, M.I.; Lapetra, J.; Zazpe, I.; et al. Adherence to a Mediterranean-type diet and reduced prevalence of clustered cardiovascular risk factors in a cohort of 3204 high-risk patients. Eur. J. Cardiovasc. Prev. Rehabil. 2008, 15, 589–593. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Schwedhelm, C.; Galbete, C.; Hoffmann, G. Adherence to Mediterranean diet and risk of cancer: An updated systematic review and meta-analysis. Nutrients 2017, 9, 1063. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.; Bryan, J.; Hodgson, J.; Murphy, K. Definition of the Mediterranean diet; a literature review. Nutrients 2015, 7, 9139–9153. [Google Scholar] [CrossRef]
- Reguant-Aleix, J.; Sensat, F. The Mediterranean diet, intangible cultural heritage of humanity. In Mediterra 2012; CIHEAM–Sciences Po Les Presses: Paris, France, 2012; pp. 465–484. [Google Scholar]
- Kittler, P.G.; Sucher, K.P.; Nelms, M. Food and Culture; Cengage Learning: Boston, MA, USA, 2011. [Google Scholar]
- Vareiro, D.; Bach-Faig, A.; Quintana, B.R.; Bertomeu, I.; Buckland, G.; de Almeida, M.D.V.; Serra-Majem, L. Availability of Mediterranean and non-Mediterranean foods during the last four decades: Comparison of several geographical areas. Public Health Nutr. 2009, 12, 1667–1675. [Google Scholar] [CrossRef] [PubMed]
- Vilarnau, C.; Stracker, D.M.; Funtikov, A.; da Silva, R.; Estruch, R.; Bach-Faig, A. Worldwide adherence to Mediterranean diet between 1960 and 2011. Eur. J. Clin. Nutr. 2019, 72, 83–91. [Google Scholar] [CrossRef]
- Rodrigues, S.; Caraher, M.; Trichopoulou, A.; De Almeida, M. Portuguese households’ diet quality (adherence to Mediterranean food pattern and compliance with WHO population dietary goals): Trends, regional disparities and socioeconomic determinants. Eur. J. Clin. Nutr. 2008, 62, 1263–1272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scott, D.M. Portuguese Americans’ acculturation, socioeconomic integration, and amalgamation: How far have they advanced? Sociol. Probl. Prat. 2009, 61, 41–64. [Google Scholar]
- Rodrigues, I.; Pan, Y.; Lubkemann, S. observing census enumeration of non-english speaking households in 2010 Census: Portuguese report. Surv. Methodol. 2013, 2013, 15. [Google Scholar]
- Pap, L. The Portuguese-Americans; Twayne Publishers: Boston, MA, USA, 1981. [Google Scholar]
- Williams, J.R. And yet they come: Portuguese Immigration from the Azores to the United States: Center for Migration Studies of New York. Can. J. Sociol. Cah. Can. Sociol. 1982, 9, 215–217. [Google Scholar]
- OECD Regional Economy [Internet]. 2015. Available online: https://www.oecd-ilibrary.org/content/data/6b288ab8-en (accessed on 30 November 2020).
- OECD Regional Education [Internet]. 2019. Available online: https://www.oecd-ilibrary.org/content/data/213e806c-en (accessed on 30 November 2020).
- Spahn, J.M.; Reeves, R.S.; Keim, K.S.; Laquatra, I.; Kellogg, M.; Jortberg, B.; Clark, N.A. State of the evidence regarding behavior change theories and strategies in nutrition counseling to facilitate health and food behavior change. J. Am. Diet. Assoc. 2010, 110, 879–891. [Google Scholar] [CrossRef]
- Prochaska, J.O.; Johnson, S.; Lee, P. The transtheoretical model of behavior change. In Handbook of Health Behavior Change; Springer Publishing Company: Washington, DC, USA, 2009. [Google Scholar]
- Mohr, P.; Quinn, S.; Morell, M.; Topping, D. Engagement with dietary fibre and receptiveness to resistant starch in Australia. Public Health Nutr. 2010, 13, 1915–1922. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weinstein, N.D.; Sandman, P.M. A model of the precaution adoption process: Evidence from home radon testing. Health Psychol. 1992, 11, 170. [Google Scholar] [CrossRef] [PubMed]
- Pollard, J.; Kirk, S.L.; Cade, J.E. Factors affecting food choice in relation to fruit and vegetable intake: A review. Nutr. Res. Rev. 2002, 15, 373–387. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teixeira, B.; Afonso, C.; Sousa, A.S.; Guerra, R.S.; Santos, A.; Borges, N.; Moreira, P.; Padrão, P.; Amaral, T.F. Adherence to a Mediterranean dietary pattern status and associated factors among Portuguese older adults: Results from the nutrition UP 65 cross-sectional study. Nutrition 2019, 65, 91–96. [Google Scholar] [CrossRef] [Green Version]
- Bottcher, M.R.; Marincic, P.Z.; Nahay, K.L.; Baerlocher, B.E.; Willis, A.W.; Park, J.; Gaillard, P.; Greene, M.W. Nutrition knowledge and Mediterranean diet adherence in the southeast United States: Validation of a field-based survey instrument. Appetite 2017, 111, 166–176. [Google Scholar] [CrossRef]
- Chen, M.; Howard, V.; Harrington, K.F.; Creger, T.; Judd, S.E.; Fontaine, K.R. Does adherence to mediterranean diet mediate the association between food environment and obesity among non-hispanic black and white older US Adults? A path analysis. Am. J. Health Promot. 2020, 34, 652–658. [Google Scholar] [CrossRef] [PubMed]
- Knight, C.J.; Jackson, O.; Rahman, I.; Burnett, D.O.; Frugé, A.D.; Greene, M.W. The Mediterranean diet in the Stroke Belt: A cross-sectional study on adherence and perceived knowledge, barriers, and benefits. Nutrients 2019, 11, 1847. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, M.K.; Mahnken, J.D.; Sullivan, D.K. NHANES 2011–2014 reveals cognition of US older adults may benefit from better adaptation to the Mediterranean diet. Nutrients 2020, 12, 1929. [Google Scholar] [CrossRef]
- Reedy, J.; Krebs-Smith, S.M.; Miller, P.E.; Liese, A.D.; Kahle, L.L.; Park, Y.; Subar, A.F. Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults. J. Nutr. 2014, 144, 881–889. [Google Scholar] [CrossRef] [Green Version]
- 2019 American Community Survey 5-Year Estimates [Internet]. 2019. Available online: https://data.census.gov/cedsci/profile?g=1600000US0680812 (accessed on 13 December 2020).
- Selected Social Characteristics in the United States, 2011–2015 American Community Survey 5-Year Estimates [Internet]. 2015. Available online: https://www1.nyc.gov/assets/planning/download/pdf/planning-level/nyc-population/acs/soc_2015acs5yr_nyc.pdf. (accessed on 29 November 2020).
- Schröder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Lamuela-Raventós, R.; Ros, E.; Lamuela-Raventos, I.; Fiol, M.; et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef] [Green Version]
- García-Conesa, M.-T.; Philippou, E.; Pafilas, C.; Massaro, M.; Quarta, S.; Andrade, V.; Jorge, R.; Chervenkov, M.; Ivanova, T.; Dimitrova, D. Exploring the validity of the 14-item Mediterranean diet adherence screener (medas): A cross-national study in seven european countries around the Mediterranean region. Nutrients 2020, 12, 2960. [Google Scholar] [CrossRef]
- Hebestreit, K.; Yahiaoui-Doktor, M.; Engel, C.; Vetter, W.; Siniatchkin, M.; Erickson, N.; Halle, M.; Kiechle, M.; Bischoff, S.C. Validation of the German version of the Mediterranean Diet Adherence Screener (MEDAS) questionnaire. BMC Cancer 2017, 17, 341. [Google Scholar] [CrossRef]
- Papadaki, A.; Johnson, L.; Toumpakari, Z.; England, C.; Rai, M.; Toms, S.; Penfold, C.; Zazpe, I.; Martínez-González, M.A.; Feder, G. Validation of the English version of the 14-item Mediterranean Diet Adherence Screener of the PREDIMED study, in people at high cardiovascular risk in the UK. Nutrients 2018, 10, 138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vaske, J.J.; Beaman, J.; Sponarski, C.C. Rethinking internal consistency in Cronbach’s alpha. Leis. Sci. 2017, 39, 163–173. [Google Scholar] [CrossRef]
- Cavaliere, A.; De Marchi, E.; Banterle, A. Exploring the adherence to the Mediterranean diet and its relationship with individual lifestyle: The role of healthy behaviors, pro-environmental behaviors, income, and education. Nutrients 2018, 10, 141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruggiero, E.; Di Castelnuovo, A.; Costanzo, S.; Persichillo, M.; Bracone, F.; Cerletti, C.; Donati, M.B.; de Gaetano, G.; Iacoviello, L.; Bonaccio, M. Socioeconomic and psychosocial determinants of adherence to the Mediterranean diet in a general adult Italian population. Eur. J. Public Health 2019, 29, 328–335. [Google Scholar] [CrossRef]
- Markides, K.S.; Rote, S. The healthy immigrant effect and aging in the United States and other western countries. Gerontologist 2019, 59, 205–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Castro, J. Education of portuguese emigrants and their acculturation. E-Methodology 2017, 4, 55–74. [Google Scholar]
- Castro, J.; Rudmin, F.W. Acculturation, acculturative change, and assimilation: A research bibliography with URL links. Online Read. Psychol. Cult. 2017, 8, 2307–0919.1075. [Google Scholar]
- Robertson, C.; Robertson, D. Portuguese Cooking: The Authentic and Robust Cuisine of Portugal. In Journal and Cookbook; North Atlantic Books: Berleley, CA, USA, 1993. [Google Scholar]
- Medina, F.X. Mediterranean diet, culture and heritage: Challenges for a new conception. Public Health Nutr. 2009, 12, 1618–1620. [Google Scholar] [CrossRef] [Green Version]
- Real, H.; Dias, R.R.; Graça, P. Mediterranean diet conceptual model and future trends of its use in Portugal. Health Promot. Int. 2020, 36, 548–560. [Google Scholar] [CrossRef] [PubMed]
- Leshem, M.; Dessie-Navon, H. Acculturation of immigrant diet, basic taste responses and sodium appetite. J. Nutr. Sci. 2018, 7, e21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haigh, L.; Bremner, S.; Houghton, D.; Henderson, E.; Avery, L.; Hardy, T.; Hallsworth, K.; McPherson, S.; Anstee, Q.M. Barriers and facilitators to Mediterranean diet adoption by patients with nonalcoholic fatty liver disease in Northern Europe. Clin. Gastroenterol. Hepatol. 2019, 17, 1364–1371. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holgado, B.; de Irala-Estevez, J.; Martinez-Gonzalez, M.; Gibney, M.; Kearney, J.; Martinez, J. Barriers and benefits of a healthy diet in Spain: Comparison with other European member states. Eur. J. Clin. Nutr. 2000, 54, 453–459. [Google Scholar] [CrossRef] [Green Version]
- Greiner, B.; Wheeler, D.; Croff, J.; Miller, B. Prior knowledge of the Mediterranean Diet is associated with dietary adherence in cardiac patients. J. Am. Osteopath Assoc. 2019, 119, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Bonaccio, M.; Bonanni, A.E.; Di Castelnuovo, A.; De Lucia, F.; Donati, M.B.; De Gaetano, G.; Iacoviello, L. Low income is associated with poor adherence to a Mediterranean diet and a higher prevalence of obesity: Cross-sectional results from the Moli-sani study. BMJ Open 2012, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Turlock † (n = 125) | Livermore † (n = 83) | ||||
|---|---|---|---|---|---|
| n | % | n | % | p-Value | |
| Sex * | 0.724 | ||||
| Male | 51 | 41 | 31 | 38 | |
| Female | 74 | 59 | 52 | 62 | |
| Age * | 0.004 | ||||
| 45–54 | 17 | 13 | 5 | 6 | |
| 55–64 | 54 | 43 | 21 | 26 | |
| 65–74 | 39 | 31 | 34 | 41 | |
| >75 | 16 | 12 | 22 | 27 | |
| Ethnicity * | 0.010 | ||||
| White | 104 | 83 | 60 | 74 | |
| Black | 5 | 4 | 4 | 5 | |
| Chinese | 0 | 0 | 9 | 9 | |
| Asian-other | 0 | 0 | 1 | 1 | |
| Other ethnic group | 17 | 13 | 9 | 11 | |
| Education * | <0.001 | ||||
| High School or lower | 61 | 61.8 | 27 | 26.8 | |
| GED | 10 | 11.4 | 4 | 3.7 | |
| Technical or trade certificate | 6 | 5.7 | 9 | 8.5 | |
| Associate’s degree | 6 | 5.7 | 24 | 24.4 | |
| Bachelor’s degree | 8 | 7.3 | 27 | 26.8 | |
| Master’s or professional degree | 10 | 8.1 | 9 | 9.8 | |
| BMI * | 0.166 | ||||
| Underweight | 1 | 0 | 2 | 2.4 | |
| Normal weight | 39 | 31.7 | 27 | 40.2 | |
| Overweight | 57 | 43.1 | 26 | 24.4 | |
| Obese | 29 | 25.2 | 27 | 32.9 | |
| Qualification * | 0.321 | ||||
| Health or nutrition related qualifications | 3 | 1.6 | 5 | 6.1 | |
| No health or nutrition related qualifications | 123 | 98.4 | 77 | 93.9 | |
| Main Effects | |||||
|---|---|---|---|---|---|
| β | SE | p-Value * | p-Value ‡ | ||
| Crude Model | |||||
| Group | Livermore | Ref † | |||
| Turlock | 0.85 | 0.26 | 0.001 | ||
| Backward Stepwise Model | |||||
| Group | 0.002 | ||||
| Livermore | Ref † | ||||
| Turlock | 0.81 | 0.30 | 0.002 | ||
| Sex | 0.030 | ||||
| Female | Ref † | ||||
| Male | −0.55 | 0.25 | 0.030 | ||
| Age | 0.043 | ||||
| 45–54 | Ref † | ||||
| 55–64 | 0.14 | 0.34 | 0.737 | ||
| 65–74 | −0.05 | 0.43 | 0.901 | ||
| >75 | 5.48 | 1.79 | 0.002 | ||
| Crude † | Adjusted †† | |||||
|---|---|---|---|---|---|---|
| Barrier | β | SE | p-Value * | β | SE | p-Value * |
| Knowledge (n = 4) ‡ (Cronbach’s Alpha = 0.43) | ||||||
| Livermore ∇ | Ref | Ref | ||||
| Turlock | 0.49 | 0.37 | 0.187 | 0.75 | 0.43 | 0.086 |
| Convenience (n = 4) (Cronbach’s Alpha = 0.76) | ||||||
| Livermore | Ref | Ref | ||||
| Turlock | 1.38 | 0.44 | 0.001 | 1.12 | 0.50 | 0.027 |
| Sensory Appeal (n = 3) (Cronbach’s Alpha = 0.75) | ||||||
| Livermore | Ref | Ref | ||||
| Turlock | 0.87 | 0.30 | 0.004 | 0.69 | 0.33 | 0.041 |
| Health (n = 4) (Cronbach’s Alpha = 0.87) | ||||||
| Livermore | Ref | Ref | ||||
| Turlock | 0.59 | 0.40 | 0.147 | 0.39 | 0.13 | 0.003 |
| Crude † | Adjusted †† | |||||
|---|---|---|---|---|---|---|
| Benefits | β | SE | p-Value * | β | SE | p-Value * |
| Health (n = 10) ‡ (Cronbach’s Alpha = 0.93) | ||||||
| Livermore∇ | Ref | Ref | ||||
| Turlock | 3.89 | 0.84 | <0.001 | 3.72 | 0.98 | <0.001 |
| Weight Loss (n = 2) (Cronbach’s Alpha = 0.63) | ||||||
| Livermore | Ref | Ref | ||||
| Turlock | 0.78 | 0.19 | <0.001 | 0.74 | 0.22 | 0.001 |
| Ethical (n = 2) (Cronbach’s Alpha = 0.89) | ||||||
| Livermore | Ref | Ref | ||||
| Turlock | 0.30 | 0.13 | 0.018 | 0.20 | 0.34 | 0.560 |
| Natural Content (n = 2) (Cronbach’s Alpha = 0.61) | ||||||
| Livermore | Ref | Ref | ||||
| Turlock | 0.57 | 0.18 | 0.001 | 0.66 | 0.20 | 0.001 |
| Familiarity (n = 2) (Cronbach’s Alpha= 0.80) | ||||||
| Livermore | Ref | Ref | ||||
| Turlock | 0.98 | 0.21 | <0.001 | 0.99 | 0.26 | <0.001 |
| Price (n = 2) (Cronbach’s Alpha = 0.91) | ||||||
| Livermore | Ref | Ref | ||||
| Turlock | 0.56 | 0.22 | 0.013 | 0.58 | 0.26 | 0.037 |
| Sensory Appeal (n = 2) (Cronbach’s Alpha = 0.79) | ||||||
| Livermore | Ref | Ref | ||||
| Turlock | 0.53 | 0.22 | 0.017 | 0.56 | 0.26 | 0.041 |
| Mood (n = 3) (Cronbach’s Alpha = 0.93) | ||||||
| Livermore | Ref | Ref | ||||
| Turlock | 1.11 | 0.34 | 0.002 | 1.01 | 0.42 | 0.017 |
| Stages of Change | Livermore | Turlock |
|---|---|---|
| Unaware/Unengaged | 67.1 | 37.4 |
| Deciding | 17.0 | 4.9 |
| Decided No | 6.1 | 0.8 |
| Decided Yes * | 4.9 | 6.5 |
| Action/Maintenance * | 4.9 | 49.6 |
| Stages of Change | |||||
|---|---|---|---|---|---|
| Unaware/Unengaged | Deciding | Decided Yes | Decided No | Action/Maintenance | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Group | |||||
| Turlock | 0.23 (0.11–0.45) *** | 0.17 (0.20–0.88) | 17.7 (6.46–64.6) *** | ||
| Sex | |||||
| Female | - | 1.55 (0.45–0.99) | - | - | - |
| Age | |||||
| 55–64 | 0.55 (0.25–1.20) | - | - | - | - |
| 65–74 | 0.54 (0.25–1.18) | 1.59 (0.68–3.64) | - | - | - |
| >75 | - | - | - | - | - |
| Ethnicity | |||||
| Black | 9.27 (1.50–180)* | - | - | - | - |
| Chinese | - | - | - | - | - |
| Asian | 3.06 (0.58–23.7) | - | - | - | - |
| Other | - | - | - | - | - |
| Education | |||||
| GED | - | - | - | 9.36 (1.13–65.3) * | - |
| Certificate | - | - | - | - | - |
| Associate’s | - | 0.40 (0.06–1.50) | - | - | - |
| Bachelor’s | 0.42 (0.16–1.04) | - | - | - | - |
| Master’s or professional | 0.20 (0.05–0.63) ** | 0.34 (0.02–1.80) | - | - | 5.59 (1.71–21.0) ** |
| BMI | |||||
| Underweight | - | - | - | - | - |
| Overweight | - | - | - | - | - |
| Obese | - | - | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Couto, R.M.; Frugé, A.D.; Greene, M.W. Adherence to the Mediterranean Diet in a Portuguese Immigrant Community in the Central Valley of California. Nutrients 2021, 13, 1989. https://doi.org/10.3390/nu13061989
Couto RM, Frugé AD, Greene MW. Adherence to the Mediterranean Diet in a Portuguese Immigrant Community in the Central Valley of California. Nutrients. 2021; 13(6):1989. https://doi.org/10.3390/nu13061989
Chicago/Turabian StyleCouto, Roberto M., Andrew D. Frugé, and Michael W. Greene. 2021. "Adherence to the Mediterranean Diet in a Portuguese Immigrant Community in the Central Valley of California" Nutrients 13, no. 6: 1989. https://doi.org/10.3390/nu13061989
APA StyleCouto, R. M., Frugé, A. D., & Greene, M. W. (2021). Adherence to the Mediterranean Diet in a Portuguese Immigrant Community in the Central Valley of California. Nutrients, 13(6), 1989. https://doi.org/10.3390/nu13061989