Estimated Prevalence and Care Pathway of Feeding and Eating Disorders in a French Pediatric Population
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Inclusion Criteria
2.3. Data Collected in the Questionnaires
2.3.1. Demographic and Medical Data
2.3.2. Age-Appropriate Dietary Behavior Questions and Additional Screening Tools
- For infants aged less than 1 year old, if the infant was fed only with milk, the type of feeding was specified (breast and/or bottle feeding), and parents completed the Baby Eating Behavior Questionnaire (BEBQ), which explores the enjoyment of food, food responsiveness, slowness in eating, satiety responsiveness and general appetite [12]. If the infant had started food, parents were asked about dietary diversification and then completed the Behavioral Pediatrics Feeding Assessment Scale (BPFAS), which evaluates the child’s behavior and the parents’ feelings about or strategies for dealing with eating problems, giving three scores (child, parent, total frequency score) [13,14]. BEBQ and BPFAS do not have a validated cut-off.
- For children aged from 1 to 12 years old, parents were asked about the child’s eating behavior and then completed the BPFAS questionnaire.
- For adolescents, parents were asked about their eating behavior, and adolescents completed three screening questionnaires: the Sick Control One Fat Food, French (SCOFF-F), which is positive when the score is ≥2 [15,16], the Eating Attitudes Test EAT-26, which is positive when the score is ≥20, and explores dieting, bulimia and oral control [17,18], they are both predictive for eating disorders, and the Three-Factor Eating Questionnaire (TFEQ-R18), which does not have a cut-off, but evaluates cognitive restriction, uncontrolled eating and emotional eating [19,20].
2.4. Classification of Disorders According to DSM-5
2.5. Statistical Analysis
3. Results
3.1. Study Sample and Demographic Data
3.2. FED Items
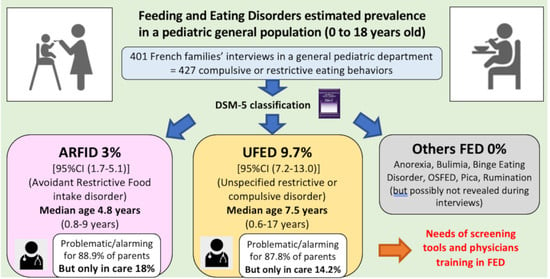
3.3. Prevalence of FED According to DSM-5
3.4. FED and BMI
3.5. FED and Analysis of Screening Tools
3.6. FED Care Pathway
4. Discussion
4.1. Prevalence of ARFID and Related Subtypes
4.2. FED Other Than ARFID
4.3. Insufficient Care of ARFID and UFED
4.4. Strength and Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 2006. [Google Scholar]
- Dahl, M.; Sundelin, C. Early Feeding Problems in an Affluent Society. Acta Paediatr. 1986, 75, 370–379. [Google Scholar] [CrossRef] [PubMed]
- Chatoor, I. Feeding disorders in infants and toddlers: Diagnosis and treatment. Child Adolesc. Psychiatr. Clin. N. Am. 2002, 11, 163–183. [Google Scholar] [CrossRef]
- Lask, B.; Bryant-Waugh, R. Early-Onset Anorexia Nervosa and Related Eating Disorders. J. Child Psychol. Psychiatry 1992, 33, 281–300. [Google Scholar] [CrossRef] [PubMed]
- Bryant-Waugh, R.; Lask, B. Overview of the eating disorders. In Eating Disorders in Childhood and Adolescence, 3rd ed.; Lask, B., Bryant-Waugh, R., Eds.; Routledge: London, UK, 2007; pp. 35–50. [Google Scholar]
- Marcus, M.D.; Kalarchian, M. Binge eating in children and adolescents. Int. J. Eat. Disord. 2003, 34, S47–S57. [Google Scholar] [CrossRef]
- Tanofsky-Kraff, M.; Goossens, L.; Eddy, K.T.; Ringham, R.; Goldschmidt, A.; Yanovski, S.Z.; Braet, C.; Marcus, M.D.; Wilfley, D.E.; Olsen, C.; et al. A multisite investigation of binge eating behaviors in children and adolescents. J. Consult. Clin. Psychol. 2007, 75, 901–913. [Google Scholar] [CrossRef] [PubMed]
- Bryant-Waugh, R.; Markham, L.; Kreipe, R.E.; Walsh, B.T. Feeding and eating disorders in childhood. Int. J. Eat. Disord. 2010, 43, 98–111. [Google Scholar] [CrossRef]
- Mammel, K.A.; Ornstein, R.M. Avoidant/restrictive food intake disorder: A new eating disorder diagnosis in the diagnostic and statistical manual 5. Curr. Opin. Pediatr. 2017, 29, 407–413. [Google Scholar] [CrossRef]
- Bryant-Waugh, R. Feeding and Eating Disorders in Children. Psychiatr. Clin. N. Am. 2019, 42, 157–167. [Google Scholar] [CrossRef] [PubMed]
- 2018 Growth Charts. Available online: https://cress-umr1153.fr/courbes-carnetdesante (accessed on 3 May 2019).
- Llewellyn, C.H.; Van Jaarsveld, C.H.; Johnson, L.; Carnell, S.; Wardle, J. Development and factor structure of the Baby Eating Behaviour Questionnaire in the Gemini birth cohort. Appetite 2011, 57, 388–396. [Google Scholar] [CrossRef]
- Crist, W.; McDonnell, P.; Beck, M.; Gillespie, C.T.; Barrett, P.; Mathews, J. Behavior at Mealtimes and the Young Child with Cystic Fibrosis. J. Dev. Behav. Pediatr. 1994, 15, 157–161. [Google Scholar] [CrossRef]
- Dovey, T.M.; Jordan, C.; Aldridge, V.K.; Martin, C.I. Screening for feeding disorders. Creating critical values using the behavioural pediatrics feeding assessment scale. Appetite 2013, 69, 108–113. [Google Scholar] [CrossRef]
- Garcia, F.D.; Grigioni, S.; Chelali, S.; Meyrignac, G.; Thibaut, F.; Déchelotte, P. Validation of the French version of SCOFF questionnaire for screening of eating disorders among adults. World J. Biol. Psychiatry 2010, 11, 888–893. [Google Scholar] [CrossRef] [PubMed]
- Garcia, F.D.; Grigioni, S.; Allais, E.; Houy-Durand, E.; Thibaut, F.; Déchelotte, P. Detection of eating disorders in patients: Validity and reliability of the French version of the SCOFF questionnaire. Clin. Nutr. 2011, 30, 178–181. [Google Scholar] [CrossRef]
- Garner, D.M.; Olmsted, M.P.; Bohr, Y.; Garfinkel, P.E. The Eating Attitudes Test: Ppsychometric features and clinical correlates. Psychol. Med. 1982, 12, 871–878. [Google Scholar] [CrossRef] [PubMed]
- Leichner, P.; Steiger, H.; Puentes-Neuman, G.; Perreault, M.; Gottheil, N. Validation d’une échelle d’attitudes alimentaires auprès d’une population québécoise francophone. Can. J. Psychiatry 1994, 39, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, J.; Persson, L.-O.; Sjöström, L.; Sullivan, M. Psychometric properties and factor structure of the Three-Factor Eating Questionnaire (TFEQ) in obese men and women. Results from the Swedish Obese Subjects (SOS) study. Int. J. Obes. 2000, 24, 1715–1725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fleurbaix Laventie Ville Sante (FLVS) Study Group; De Lauzon, B.; Romon, M.; Deschamps, V.; Lafay, L.; Borys, J.-M.; Karlsson, J.; Ducimetière, P.; Charles, M.A. The Three-Factor Eating Questionnaire-R18 Is Able to Distinguish among Different Eating Patterns in a General Population. J. Nutr. 2004, 134, 2372–2380. [Google Scholar] [CrossRef]
- Demographic Review. 2019. Available online: https://www.insee.fr/fr/statistiques/1892088?sommaire=1912926. (accessed on 5 July 2020).
- Mohammadi, M.R.; Mostafavi, S.; Hooshyari, Z.; Khaleghi, A.; Ahmadi, N.; Molavi, P.; Kian, A.A.; Safavi, P.; Delpisheh, A.; Talepasand, S.; et al. Prevalence, correlates and comorbidities of feeding and eating disorders in a nationally representative sample of Iranian children and adolescents. Int. J. Eat. Disord. 2020, 53, 349–361. [Google Scholar] [CrossRef] [PubMed]
- Galmiche, M.; Déchelotte, P.; Lambert, G.; Tavolacci, M.P. Prevalence of eating disorders over the 2000–2018 period: A systematic literature review. Am. J. Clin. Nutr. 2019, 109, 1402–1413. [Google Scholar] [CrossRef]
- Hay, P.; Mitchison, D.; Collado, A.E.L.; González-Chica, D.A.; Stocks, N.; Touyz, S. Burden and health-related quality of life of eating disorders, including Avoidant/Restrictive Food Intake Disorder (ARFID), in the Australian population. J. Eat. Disord. 2017, 5, 1–10. [Google Scholar] [CrossRef]
- Silén, Y.; Sipilä, P.N.; Raevuori, A.; Mustelin, L.; Marttunen, M.; Kaprio, J.; Keski-Rahkonen, A. DSM-5 eating disorders among adolescents and young adults in Finland: A public health concern. Int. J. Eat. Disord. 2020, 53, 790–801. [Google Scholar] [CrossRef] [PubMed]
- Krom, H.; Veer, L.V.D.S.; Van Zundert, S.; Otten, M.; Benninga, M.; Haverman, L.; Kindermann, A. Health related quality of life of infants and children with avoidant restrictive food intake disorder. Int. J. Eat. Disord. 2019, 52, 410–418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cooney, M.; Lieberman, M.; Guimond, T.; Katzman, D.K. Clinical and psychological features of children and adolescents diagnosed with avoidant/restrictive food intake disorder in a pediatric tertiary care eating disorder program: A descriptive study. J. Eat. Disord. 2018, 6, 7. [Google Scholar] [CrossRef] [PubMed]
- Eddy, K.T.; Thomas, J.J.; Bs, E.H.; Ba, K.E.; Lamont, E.; Ba, C.M.N.; Ba, R.M.P.; Ba, H.B.M.; Bryant-Waugh, R.; Becker, A.E. Prevalence of DSM-5 avoidant/restrictive food intake disorder in a pediatric gastroenterology healthcare network. Int. J. Eat. Disord. 2015, 48, 464–470. [Google Scholar] [CrossRef] [PubMed]
- A Nicely, T.; Lane-Loney, S.; Masciulli, E.; Hollenbeak, C.S.; Ornstein, R.M. Prevalence and characteristics of avoidant/restrictive food intake disorder in a cohort of young patients in day treatment for eating disorders. J. Eat. Disord. 2014, 2, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Fisher, M.M.; Rosen, D.S.; Ornstein, R.M.; Mammel, K.A.; Katzman, D.K.; Rome, E.S.; Callahan, S.T.; Malizio, J.; Kearney, S.; Walsh, B.T. Characteristics of Avoidant/Restrictive Food Intake Disorder in Children and Adolescents: A “New Disorder” in DSM-5. J. Adolesc. Heal. 2014, 55, 49–52. [Google Scholar] [CrossRef] [Green Version]
- Norris, M.L.; Robinson, A.; Obeid, N.; Harrison, M.; Spettigue, W.; Henderson, K. Exploring avoidant/restrictive food intake disorder in eating disordered patients: A descriptive study. Int. J. Eat. Disord. 2014, 47, 495–499. [Google Scholar] [CrossRef]
- Kurz, S.; Van Dyck, Z.; Dremmel, D.; Munsch, S.; Hilbert, A. Early-onset restrictive eating disturbances in primary school boys and girls. Eur. Child Adolesc. Psychiatry 2015, 24, 779–785. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.-L.; Chen, W.J.; Lin, K.-C.; Shen, L.-J.; Gau, S.S.-F. Prevalence of DSM-5 mental disorders in a nationally representative sample of children in Taiwan: Methodology and main findings. Epidemiology Psychiatr. Sci. 2019, 29, 1–9. [Google Scholar] [CrossRef]
- Goldberg, H.R.; Katzman, D.K.; Allen, L.; Martin, S.; Sheehan, C.; Kaiserman, J.; Macdonald, G.; Kives, S. The Prevalence of Children and Adolescents at Risk for Avoidant Restrictive Food Intake Disorder in a Pediatric and Adolescent Gynecology Clinic. J. Pediatr. Adolesc. Gynecol. 2020, 33, 466–469. [Google Scholar] [CrossRef]
- Schöffel, H.; Hiemisch, A.; Kiess, W.; Hilbert, A.; Schmidt, R. Characteristics of avoidant/restrictive food intake disorder in a general paediatric inpatient sample. Eur. Eat. Disord. Rev. 2021, 29, 60–73. [Google Scholar] [CrossRef] [PubMed]
- Benjasuwantep, B.; Chaithirayanon, S.; Eiamudomkan, M. Feeding Problems in Healthy Young Children: Prevalence, Related Factors and Feeding Practices. Pediatr. Rep. 2013, 5, 38–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, C.M.; Wernimont, S.M.; Northstone, K.; Emmett, P.M. Picky/fussy eating in children: Review of definitions, assessment, prevalence and dietary intakes. Appetite 2015, 95, 349–359. [Google Scholar] [CrossRef] [Green Version]
- Sarin, H.V.; Taba, N.; Fischer, K.; Esko, T.; Kanerva, N.; Moilanen, L.; Saltevo, J.; Joensuu, A.; Borodulin, K.; Männistö, S.; et al. Food neophobia associates with poorer dietary quality, metabolic risk factors, and increased disease outcome risk in population-based cohorts in a metabolomics study. Am. J. Clin. Nutr. 2019, 110, 233–245. [Google Scholar] [CrossRef]
- Kovacic, K.; Rein, S.L.E.; Szabo, A.; Kommareddy, S.; Bhagavatula, P.; Goday, P.S. Pediatric Feeding Disorder: A Nationwide Prevalence Study. J. Pediatr. 2021, 228, 126–131.e3. [Google Scholar] [CrossRef] [PubMed]
- Rosen, R. Prevalence of Feeding Disorders: A Tough Reality to Swallow. J. Pediatr. 2021, 228, 13–14. [Google Scholar] [CrossRef]
- Machado, P.P.; Ma, B.C.M.; Gonçalves, S.; Hoek, H.W.; Machado, B.C. The prevalence of eating disorders not otherwise specified. Int. J. Eat. Disord. 2007, 40, 212–217. [Google Scholar] [CrossRef]
- Nicholls, D.E.; Lynn, R.M.; Viner, R.M. Childhood eating disorders: British national surveillance study. Br. J. Psychiatry 2011, 198, 295–301. [Google Scholar] [CrossRef] [Green Version]
- Bohon, C. Binge Eating Disorder in Children and Adolescents. Child Adolesc. Psychiatr. Clin. N. Am. 2019, 28, 549–555. [Google Scholar] [CrossRef]
- Hartmann, A.S.; Poulain, T.; Vogel, M.; Hiemisch, A.; Kiess, W.; Hilbert, A. Prevalence of pica and rumination behaviors in German children aged 7–14 and their associations with feeding, eating, and general psychopathology: A population-based study. Eur. Child Adolesc. Psychiatry 2018, 27, 1499–1508. [Google Scholar] [CrossRef]
- Ba, H.B.M.; Thomas, J.J.; Hinz, A.; Munsch, S.; Hilbert, A. Prevalence in primary school youth of pica and rumination behavior: The understudied feeding disorders. Int. J. Eat. Disord. 2018, 51, 994–998. [Google Scholar] [CrossRef] [Green Version]
- Hail, L.; Le Grange, D. Bulimia nervosa in adolescents: Prevalence and treatment challenges. Adolesc. Heal. Med. Ther. 2018, 9, 11–16. [Google Scholar] [CrossRef] [Green Version]
- He, J.; Cai, Z.; Fan, X. Prevalence of binge and loss of control eating among children and adolescents with overweight and obesity: An exploratory meta-analysis. Int. J. Eat. Disord. 2017, 50, 91–103. [Google Scholar] [CrossRef] [PubMed]
- Suri, S.; Pradhan, R. Assessment of Night Eating Syndrome Among Late Adolescents. Indian J. Psychol. Med. 2010, 32, 71–72. [Google Scholar] [CrossRef] [Green Version]
- Lamerz, A.; Kuepper-Nybelen, J.; Bruning, N.; Wehle, C.; Trost-Brinkhues, G.; Brenner, H.; Hebebrand, J.; Herpertz-Dahlmann, B. Prevalence of obesity, binge eating, and night eating in a cross-sectional field survey of 6-year-old children and their parents in a German urban population. J. Child Psychol. Psychiatry 2005, 46, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Ornstein, R.M.; Rosen, D.S.; Mammel, K.A.; Callahan, S.T.; Forman, S.; Jay, M.S.; Fisher, M.; Rome, E.; Walsh, B.T. Distribution of Eating Disorders in Children and Adolescents Using the Proposed DSM-5 Criteria for Feeding and Eating Disorders. J. Adolesc. Heal. 2013, 53, 303–305. [Google Scholar] [CrossRef] [PubMed]
- Forman, S.F.; McKenzie, N.; Hehn, R.; Monge, M.C.; Kapphahn, C.J.; Mammel, K.A.; Callahan, S.T.; Sigel, E.J.; Bravender, T.; Romano, M.; et al. Predictors of Outcome at 1 Year in Adolescents With DSM-5 Restrictive Eating Disorders: Report of the National Eating Disorders Quality Improvement Collaborative. J. Adolesc. Heal. 2014, 55, 750–756. [Google Scholar] [CrossRef] [PubMed]
- Strandjord, S.E.; Sieke, E.H.; Richmond, M.; Rome, E.S. Avoidant/Restrictive Food Intake Disorder: Illness and Hospital Course in Patients Hospitalized for Nutritional Insufficiency. J. Adolesc. Heal. 2015, 57, 673–678. [Google Scholar] [CrossRef]
- Zimmerman, J.; Fisher, M. Avoidant/Restrictive Food Intake Disorder (ARFID). Curr. Probl. Pediatr. Adolesc. Heal. Care 2017, 47, 95–103. [Google Scholar] [CrossRef]
- Rommel, N.; De Meyer, A.-M.; Feenstra, L.; Veereman-Wauters, G. The Complexity of Feeding Problems in 700 Infants and Young Children Presenting to a Tertiary Care Institution. J. Pediatr. Gastroenterol. Nutr. 2003, 37, 75–84. [Google Scholar] [CrossRef]
- Kerzner, B.; Milano, K.; MacLean, W.C.; Berall, G.; Stuart, S.; Chatoor, I. A Practical Approach to Classifying and Managing Feeding Difficulties. Pediatr. 2015, 135, 344–353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borowitz, K.C.; Borowitz, S.M. Feeding Problems in Infants and Children. Pediatr. Clin. N. Am. 2018, 65, 59–72. [Google Scholar] [CrossRef] [PubMed]
- Goday, P.S.; Huh, S.Y.; Silverman, A.; Lukens, C.T.; Dodrill, P.; Cohen, S.S.; Delaney, A.L.; Feuling, M.B.; Noel, R.J.; Gisel, E.; et al. Pediatric Feeding Disorder. J. Pediatr. Gastroenterol. Nutr. 2019, 68, 124–129. [Google Scholar] [CrossRef]
- Milano, K.; Chatoor, I.; Kerzner, B. A Functional Approach to Feeding Difficulties in Children. Curr. Gastroenterol. Rep. 2019, 21, 51. [Google Scholar] [CrossRef]
- Aviram, I.; Atzaba-Poria, N.; Pike, A.; Meiri, G.; Yerushalmi, B. Mealtime Dynamics in Child Feeding Disorder: The Role of Child Temperament, Parental Sense of Competence, and Paternal Involvement. J. Pediatr. Psychol. 2014, 40, 45–54. [Google Scholar] [CrossRef] [Green Version]
- Herle, M.; De Stavola, B.; Hübel, C.; Abdulkadir, M.; Ferreira, D.L.S.; Loos, R.; Bryant-Waugh, R.; Bulik, C.M.; Micali, N. A longitudinal study of eating behaviours in childhood and later eating disorder behaviours and diagnoses. Br. J. Psychiatry 2019, 216, 113–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Katzman, D.K.; Stevens, K.; Norris, M. Redefining feeding and eating disorders: What is avoidant/restrictive food intake disorder? Paediatr. Child Heal. 2014, 19, 445–446. [Google Scholar] [CrossRef] [Green Version]
- Schmidt, R.; Kirsten, T.; Hiemisch, A.; Kiess, W.; Hilbert, A. Interview-based assessment of avoidant/restrictive food intake disorder (ARFID): A pilot study evaluating an ARFID module for the Eating Disorder Examination. Int. J. Eat. Disord. 2019, 52, 388–397. [Google Scholar] [CrossRef]
- Bryant-Waugh, R.; Micali, N.; Cooke, L.; Lawson, E.A.; Eddy, K.T.; Thomas, J.J. Development of the Pica, ARFID, and Rumination Disorder Interview, a multi-informant, semi-structured interview of feeding disorders across the lifespan: A pilot study for ages 10–22. Int. J. Eat. Disord. 2019, 52, 378–387. [Google Scholar] [CrossRef]
- Total Births by Sex. Available online: https://www.ined.fr/fr/tout-savoir-population/chiffres/france/naissance-fecondite/naissances-sexe/ (accessed on 6 September 2020).
- Vanhelst, J.; Baudelet, J.-B.; Thivel, D.; Ovigneur, H.; Deschamps, T. Trends in the prevalence of overweight, obesity and underweight in French children, aged 4–12 years, from 2013 to 2017. Public Heal. Nutr. 2020, 23, 2478–2484. [Google Scholar] [CrossRef] [PubMed]
- Garrido-Miguel, M.; Cavero-Redondo, I.; Álvarez-Bueno, C.; Rodriguez-Artalejo, F.; Aznar, L.M.; Ruiz, J.R.; Martinez-Vizcaino, V. Prevalence and trends of thinness, overweight and obesity among children and adolescents aged 3–18 years across Europe: A protocol for a systematic review and meta-analysis. BMJ Open 2017, 7, e018241. [Google Scholar] [CrossRef] [PubMed]
- Byrne, R.; Jansen, E.; Daniels, L. Perceived fussy eating in Australian children at 14 months of age and subsequent use of maternal feeding practices at 2 years. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 123. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Age Groups (Total n = 401 Patients) | |||||
|---|---|---|---|---|---|
| 0–1 Year Old n = 101 | 1–6 Years Old n = 99 | 6–12 Years Old n = 100 | 12–18 Years Old n = 101 | p * | |
| Sex ratio | 1.2 | 0.86 | 1.2 | 1.1 | 0.58 |
| Median age (min-max) | 3.5 months (0.1–11.9) | 3 years old (1–5.5) | 8 years old (6–11.5) | 14 years old (12–18) | |
| BMI overweight (including obesity) | 8.9% | 15.1% | 28% | 28.7% | <0.001 |
| BMI grade II underweight | 1.9% | 12.1% | 4% | 0% | <0.001 |
| Age Groups (Total n = 401 Patients, 427 FED Items) | |||||
|---|---|---|---|---|---|
| n = FED Item/Patient (%) | 0–1 Year Old n = 101 Infants n = 23 Items | 1–6 Years Old n = 99 Children n = 112 Items | 6–12 Years Old n = 100 Children n = 133 Items | 12–18 Years Old n = 101 Adolescents n = 159 Items | p (χ2 Test) |
| Breastfeeding withdrawal problems n = 2/31(6.4%) | 2/31 breast-feeding (6.4%) | 0/99 (0%) | NA | NA | NA |
| Difficulty taking the bottle n = 0 (0%) | 0/101 (0%) | 0/99 (0%) | NA | NA | NA |
| Refusal of the spoon n = 2/142 (1.4%) | 2/43 infants who had started food (4.6%) | 0/99 (0%) | NA | NA | NA |
| Refusal of pieces n = 10/343 (2.9%) | 4/43 infants who had started food (9.3%) | 6/99 (6%) | 0/100 (0%) | 0/101 (0%) | 0.004 |
| Picky eater n = 66/401 (16.4%) | 6/101 (6%) | 30/99 (30%) | 17/100 (17%) | 13/101 (13%) | <0.001 |
| Neophobic/selective eater n = 22/343 (6.4%) | 1/43 infants who had started food (2.3%) | 7/99 (7%) | 9/100 (9%) | 5/101 (5%) | 0.57 |
| Restrictive eater n = 7/343 (2%) | 0/101 (0%) | 6/99 (6%) | 1/100 (1%) | 0/101 (0%) | 0.01 |
| Phobia of swallowing and/or vomiting n = 4/300 (1.3%) | NA | 3/99 (3%) | 1/100 (1%) | 0/101 (0%) | 0.16 |
| Emotional food avoidance n = 1/300 (0.3%) | NA | 0/99 (0%) | 1/100 (1%) | 0/101 (0%) | NA |
| Big eater n = 93/401 (23.2%) | 8/101 (8%) | 25/99 (25%) | 29/100 (29%) | 31/101 (31%) | 0.001 |
| Hyperphagia n = 20/343 (5.8%) | NA | 0/99 (0%) | 8/100 (8%) | 12/101 (12%) | 0.003 |
| Compulsive eating n = 5/343 (1.4%) | NA | 0/99 (0%) | 1/100 (1%) | 4/101 (4%) | 0.07 |
| Nocturnal nibbling n = 4/343 (1.1%) | NA | 0/99 (0%) | 0/100 (0%) | 4/101 (4%) | 0.02 |
| Nocturnal hyperphagia n = 1/343 (0.3%) | NA | 0/99 (0%) | 0/100 (0%) | 1/101 (1%) | 0.37 |
| Tachyphagia n = 101/343 (29.4%) | NA | 21/99 (21%) | 30/100 (30%) | 50/101 (50%) | <0.001 |
| Nibbling between meals n = 89/343 (25.9%) | NA | 14/99 (14%) | 36/100 (36%) | 39/101 (39%) | <0.001 |
| Anorexia or bulimia nervosa, binge eating disorder, rumination, pica, orthorexia n = 0/300 | NA | 0/99 (0%) | 0/100 (0%) | 0/101 (0%) | NA |
| Age Groups (Total n = 401 Patients) | |||||
|---|---|---|---|---|---|
| DSM-5 FED n = 46/401 (11.4%) | 0–1 Year Old n = 101 | 1–6 Years Old n = 99 | 6–12 Years Old n = 100 | 12–18 Years Old n = 101 | p (χ2 Test) |
| ARFID n = 11/401 (2.7%) | n = 1 (1%) | n = 6 (6%) | n = 4 (4%) | n = 0 | |
| Selective n = 3 (including 1 refusal of pieces) | 1 | 0 | 2 | 0 | 0.09 |
| Emotional food avoidance n = 1 | 0 | 0 | 1 | 0 | |
| Restrictive eater n = 7 (including 1phobia SV, 3 selective eaters) | 0 | 6 | 1 | 0 | |
| Unspecified FED n = 35/401 (8.7%) | n = 6 (6%) | n = 8 (8%) | n = 9 (9%) | n = 12 (12%) | |
| Compulsive eating n = 4 | 0 | 0 | 1 | 3 | |
| Nocturnal snacking/hyperphagia n = 5 (including 1 selective) | 0 | 0 | 0 | 5 | |
| Refusal of pieces + phobia SV n = 1 | 0 | 1 | 0 | 0 | |
| Refusal of pieces + selective n = 2 | 0 | 2 | 0 | 0 | |
| Selective eater n = 12 | 0 | 1 | 7 | 4 | |
| Phobia SV + selective eater n = 1 | 0 | 1 | 0 | 0 | |
| Phobia SV n = 1 | 0 | 0 | 1 | 0 | |
| Refusal of pieces n = 6 | 3 | 3 | 0 | 0 | |
| Refusal of the spoon n = 1 | 1 | 0 | 0 | 0 | |
| Breastfeeding withdrawal problem n = 1 | 1 | 0 | - | - | |
| Refusal of the spoon + breastfeeding withdrawal problem n = 1 | 1 | 0 | - | - | |
| Anorexia nervosa, bulimia nervosa, binge eating disorder, rumination, pica, other specified FED n = 0 | 0 | 0 | 0 | 0 | |
| Age Groups (Total n = 401 Patients) | |||||
|---|---|---|---|---|---|
| Parents’ Feelings | 0–1 Year Old n = 101 | 1–6 Years Old n = 99 | 6–12 Years Old n = 100 | 12–18 Years Old n = 101 | p |
| Having a child with current eating difficulties (20%) | 11.0% | 20.0% | 19.0% | 30.0% | 0.021 |
| Perception of the child’s eating difficulties | <0.001 | ||||
| It is not a problem (20.3%) | 18.2% | 17.6% | 23.5% | 20.7% | |
| It is a problem (52.7%) | 45.4% | 64.7% | 52.9% | 48.3% | |
| It is alarming (27%) | 36.4% | 17.6% | 23.5% | 31.0% | |
| Child receiving professional care (22.3%) | 54.5% | 15.0% | 15.8% | 26.9% | 0.007 |
| General practitioner (29.4%) | 66.7% | 33.3% | 66.7% | - | |
| Pediatrician (35.2%) | 33.3% | 66.7% | - | 28.6% | |
| Psychiatrist (5.9%) | - | - | - | 28.6% | |
| Dietician (11.7%) | - | - | 33.3% | 42.8% | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bertrand, V.; Tiburce, L.; Sabatier, T.; Dufour, D.; Déchelotte, P.; Tavolacci, M.-P. Estimated Prevalence and Care Pathway of Feeding and Eating Disorders in a French Pediatric Population. Nutrients 2021, 13, 2048. https://doi.org/10.3390/nu13062048
Bertrand V, Tiburce L, Sabatier T, Dufour D, Déchelotte P, Tavolacci M-P. Estimated Prevalence and Care Pathway of Feeding and Eating Disorders in a French Pediatric Population. Nutrients. 2021; 13(6):2048. https://doi.org/10.3390/nu13062048
Chicago/Turabian StyleBertrand, Valérie, Lyvia Tiburce, Thibaut Sabatier, Damien Dufour, Pierre Déchelotte, and Marie-Pierre Tavolacci. 2021. "Estimated Prevalence and Care Pathway of Feeding and Eating Disorders in a French Pediatric Population" Nutrients 13, no. 6: 2048. https://doi.org/10.3390/nu13062048
APA StyleBertrand, V., Tiburce, L., Sabatier, T., Dufour, D., Déchelotte, P., & Tavolacci, M. -P. (2021). Estimated Prevalence and Care Pathway of Feeding and Eating Disorders in a French Pediatric Population. Nutrients, 13(6), 2048. https://doi.org/10.3390/nu13062048