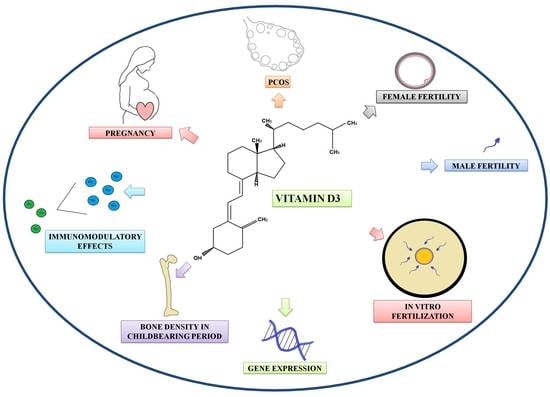
Effects of Vitamin D on Fertility, Pregnancy and Polycystic Ovary Syndrome—A Review
Abstract
:1. Introduction
2. Materials and Methods
3. Influence of Vitamin D on Fertility and In Vitro Fertilization
4. Polycystic Ovary Syndrome and Vitamin D Deficiency
5. Vitamin D Deficiency and Pregnancy
6. Vitamin D Deficiency and Female Bone Mineral Density (BMD) in Childbearing Period and Pregnancy-Related Transient Osteoporosis of the Hip
| Study | Article Type | Study Group | Summary |
|---|---|---|---|
| Ó Breasail et al. [92] | Case control study | Healthy pregnant women (n = 53), non-pregnant and non-lactating (n = 37) | Significant decrease in volumetric bone mineral density and a different pattern of microarchitecture were seen mainly in the tibia (not in radius) in the pregnant group, suggesting compartment-specific maternal bone mineral density and microarchitecture changes during pregnancy. |
| Moller et al. [91] | Controlled cohort study | Women planning pregnancy (in total 153 women, conceived n = 92), women in postpartum (19 month, n = 31) and age-matched controls (n = 75) | Pregnancy and breastfeeding also lead to reversible bone loss, which returns to pre-pregnancy levels 19 months after delivery, independent of the length of breastfeeding. |
| Steib-Furno et al. [99] | Prospective survey and retrospective study | Pregnant women (n = 4900) | Pregnancy-related transient osteoporosis of the hip (PR-TOH) is a rare, benign orthopedic–obstetrical illness, it usually occurs during the third trimester of pregnancy. |
| Curtis et al. [93] | Randomized controlled trial | Pregnant women (Placebo group (n = 188), cholecalciferol-supplemented (n = 184)) | The bone resorption marker urinary C-terminal telopeptide of type I collagen (CTX) increased during pregnancy. This occurred to a lesser extent during vitamin D supplementation during pregnancy and this was inversely associated with maternal bone mass following delivery. These results may indicate that vitamin D supplementation may ameliorate and prevent pregnancy-related reversible bone loss in mothers. |
7. Comparability of Vitamin D Studies
8. Summary and Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Thomson, R.L.; Spedding, S.; Buckley, J.D. Vitamin D in the aetiology and management of polycystic ovary syndrome. Clin. Endocrinol. 2012, 77, 343–350. [Google Scholar] [CrossRef]
- Muscogiuri, G.; Altieri, B.; Annweiler, C.; Balercia, G.; Pal, H.B.; Boucher, B.J.; Cannell, J.J.; Foresta, C.; Grübler, M.R.; Kotsa, K.; et al. Vitamin D and chronic diseases: The current state of the art. Arch. Toxicol. 2017, 91, 97–107. [Google Scholar] [CrossRef]
- Muscogiuri, G.; Altieri, B.; de Angelis, C.; Palomba, S.; Pivonello, R.; Colao, A.; Orio, F. Shedding new light on female fertility: The role of vitamin D. Rev. Endocr. Metab. Disord. 2017, 18, 273–283. [Google Scholar] [CrossRef]
- Rak, K.; Bronkowska, M. Immunomodulatory Effect of Vitamin D and Its Potential Role in the Prevention and Treatment of Type 1 Diabetes Mellitus—A Narrative Review. Molecules 2018, 24, 53. [Google Scholar] [CrossRef] [Green Version]
- Bouillon, R.; Carmeliet, G.; Verlinden, L.; van Etten, E.; Verstuyf, A.; Luderer, H.F.; Lieben, L.; Mathieu, C.; DeMay, M. Vitamin D and Human Health: Lessons from Vitamin D Receptor Null Mice. Endocr. Rev. 2008, 29, 726–776. [Google Scholar] [CrossRef]
- Fetahu, I.; Höbaus, J.; Kállay, E. Vitamin D and the epigenome. Front. Physiol. 2014, 5, 164. [Google Scholar] [CrossRef] [Green Version]
- Bird, A. DNA methylation and the frequency of CpG in animal DNA. Nucleic Acids Res. 1980, 8, 1499–1504. [Google Scholar] [CrossRef]
- Gruenbaum, Y.; Stein, R.; Cedar, H.; Razin, A. Methylation of CpG sequences in eukaryotic DNA. FEBS Lett. 1981, 124, 67–71. [Google Scholar] [CrossRef] [Green Version]
- Tapp, H.S.; Commane, D.; Bradburn, D.M.; Arasaradnam, R.; Mathers, J.C.; Johnson, I.; Belshaw, N.J. Nutritional factors and gender influence age-related DNA methylation in the human rectal mucosa. Aging Cell 2012, 12, 148–155. [Google Scholar] [CrossRef]
- Zhu, H.; Wang, X.; Shi, H.; Su, S.; Harshfield, G.A.; Gutin, B.; Snieder, H.; Dong, Y. A Genome-Wide Methylation Study of Severe Vitamin D Deficiency in African American Adolescents. J. Pediatr. 2013, 162, 1004–1009.e1. [Google Scholar] [CrossRef] [Green Version]
- López-Otín, C.; Blasco, M.A.; Partridge, L.; Serrano, M.; Kroemer, G. The hallmarks of aging. Cell 2013, 153, 1194–1217. [Google Scholar] [CrossRef] [Green Version]
- Jylhävä, J.; Pedersen, N.L.; Hägg, S. Biological Age Predictors. EBioMedicine 2017, 21, 29–36. [Google Scholar] [CrossRef] [Green Version]
- Vetter, V.M.; Sommerer, Y.; Kalies, C.H.; Spira, D.; Bertram, L.; Demuth, I. Vitamin D Supplementation is Associated with Slower Epigenetic Aging. MedRxiv 2021. [Google Scholar] [CrossRef]
- Holick, M.F. The vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention. Rev. Endocr. Metab. Disord. 2017, 18, 153–165. [Google Scholar] [CrossRef]
- Takács, I.; Dank, M.; Majnik, J.; Nagy, G.; Szabó, A.; Szabó, B.; Szekanecz, Z.; Sziller, I.; Toldy, E.; Tislér, A.; et al. Magyarországi konszenzusajánlás a D-vitamin szerepéről a betegségek megelőzésében és kezelésében. Orv. Hetil. 2022, 15, 575–584. [Google Scholar] [CrossRef]
- Franasiak, J.M.; Lara-Molina, E.E.; Pellicer, A. Vitamin D in human reproduction. Curr. Opin. Obstet. Gynecol. 2017, 29, 189–194. [Google Scholar] [CrossRef]
- Nandi, A.; Sinha, N.; Ong, E.; Sonmez, H.; Poretsky, L. Is there a role for vitamin D in human reproduction? Horm. Mol. Biol. Clin. Investig. 2016, 25, 15–28. [Google Scholar] [CrossRef]
- Voulgaris, N.; Papanastasiou, L.; Piaditis, G.; Angelousi, A.; Kaltsas, G.; Mastorakos, G.; Kassi, E. Vitamin D and aspects of female fertility. Hormones 2017, 16, 5–21. [Google Scholar] [CrossRef] [Green Version]
- Dennis, N.; Houghton, L.; Jones, G.T.; Van Rij, A.M.; Morgan, K.; McLennan, I.S. The Level of Serum Anti-Müllerian Hormone Correlates with Vitamin D Status in Men and Women but Not in Boys. J. Clin. Endocrinol. Metab. 2012, 97, 2450–2455. [Google Scholar] [CrossRef] [Green Version]
- Rojansky, N.; Brzezinski, A.; Schenker, J. Seasonality in human reproduction: An update. Hum. Reprod. 1992, 7, 735–745. [Google Scholar] [CrossRef]
- Kinuta, K.; Tanaka, H.; Moriwake, T.; Aya, K.; Kato, S.; Seino, Y. Vitamin D is an important factor in estrogen biosynthesis of both female and male gonads. Endocrinology 2000, 141, 1317–1324. [Google Scholar] [CrossRef]
- Akhavizadegan, H.; Karbakhsh, M. Comparison of Serum Vitamin D between Fertile and Infertile Men in A Vitamin D Deficient Endemic Area: A Case-Control Study. Urol. J. 2017, 84, 218–220. [Google Scholar] [CrossRef]
- Lorenzen, M.; Boisen, I.M.; Mortensen, L.J.; Lanske, B.; Juul, A.; Jensen, M.B. Reproductive endocrinology of vitamin D. Mol. Cell. Endocrinol. 2017, 453, 103–112. [Google Scholar] [CrossRef]
- Ozkan, S.; Jindal, S.; Greenseid, K.; Shu, J.; Zeitlian, G.; Hickmon, C.; Pal, L. Replete vitamin D stores predict reproductive success following in vitro fertilization. Fertil. Steril. 2010, 94, 1314–1319. [Google Scholar] [CrossRef] [Green Version]
- Xu, J.; Hennebold, J.D.; Seifer, D.B. Direct vitamin D3 actions on rhesus macaque follicles in three-dimensional culture: Assessment of follicle survival, growth, steroid, and antimüllerian hormone production. Fertil. Steril. 2016, 106, 1815–1820.e1. [Google Scholar] [CrossRef] [Green Version]
- Azziz, R. Polycystic Ovary Syndrome. Obs. Gynecol. 2018, 132, 321–336. [Google Scholar] [CrossRef]
- March, W.A.; Moore, V.M.; Willson, K.J.; Phillips, D.I.; Norman, R.; Davies, M.J. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum. Reprod. 2009, 25, 544–551. [Google Scholar] [CrossRef] [Green Version]
- Pal, L.; Zhang, H.; Williams, J.; Santoro, N.F.; Diamond, M.P.; Schlaff, W.D.; Coutifaris, C.; Carson, S.A.; Steinkampf, M.P.; Carr, B.R.; et al. Vitamin D Status Relates to Reproductive Outcome in Women with Polycystic Ovary Syndrome: Secondary Analysis of a Multicenter Randomized Controlled Trial. J. Clin. Endocrinol. Metab. 2016, 101, 3027–3035. [Google Scholar] [CrossRef]
- Goodarzi, M.O.; Dumesic, D.A.; Chazenbalk, G.; Azziz, R. Polycystic ovary syndrome: Etiology, pathogenesis and diagnosis. Nat. Rev. Endocrinol. 2011, 7, 219–231. [Google Scholar] [CrossRef]
- Szydlarska, D.; Machaj, M.; Jakimiuk, A. History of discovery of polycystic ovary syndrome. Adv. Clin. Exp. Med. 2017, 26, 555–558. [Google Scholar] [CrossRef] [Green Version]
- Han, F.F.; Lv, Y.L.; Gong, L.L.; Liu, H.; Wan, Z.R.; Liu, L.H. VDR Gene variation and insulin resistance related diseases. Lipids Health Dis. 2017, 16, 157. [Google Scholar] [CrossRef] [Green Version]
- Zadeh-Vakili, A.; Tehrani, F.R.; Daneshpour, M.A.; Zarkesh, M.; Saadat, N.; Azizi, F. Genetic polymorphism of vitamin D receptor gene affects the phenotype of PCOS. Gene 2013, 515, 193–196. [Google Scholar] [CrossRef]
- Mu, Y.; Cheng, D.; Yin, T.-L.; Yang, J. Vitamin D and Polycystic Ovary Syndrome: A Narrative Review. Reprod. Sci. 2021, 28, 2110–2117. [Google Scholar] [CrossRef]
- Kuyucu, Y.; Çelik, L.S.; Kendirlinan, Ö.; Tap, Özgül; Mete, U.Ö. Investigation of the uterine structural changes in the experimental model with polycystic ovary syndrome and effects of vitamin D treatment: An ultrastructural and immunohistochemical study. Reprod. Biol. 2018, 18, 53–59. [Google Scholar] [CrossRef]
- Tannus, S.; Tan, J.; Son, W.Y.; Dahan, M. Prevalence, clinical characteristics, and reproductive outcomes of polycystic ovary syndrome in older women referred for tertiary fertility care. Arch. Gynecol. Obstet. 2017, 297, 1037–1042. [Google Scholar] [CrossRef]
- Guo, J.; Liu, S.; Wang, P.; Ren, H.; Li, Y. Characterization of VDR and CYP27B1 expression in the endometrium during the menstrual cycle before embryo transfer: Implications for endometrial receptivity. Reprod. Biol. Endocrinol. 2020, 18, 24. [Google Scholar] [CrossRef]
- Menichini, D.; Forte, G.; Orrù, B.; Gullo, G.; Unfer, V.; Facchinetti, F. The role of vitamin D in metabolic and reproductive disturbances of polycystic ovary syndrome: A narrative mini-review. Int. J. Vitam. Nutr. Res. 2020, 92, 126–133. [Google Scholar] [CrossRef]
- Aghadavod, E.; Mollaei, H.; Nouri, M.; Hamishehkar, H. Evaluation of Relationship between Body Mass Index with Vitamin D Receptor Gene Expression and Vitamin D Levels of Follicular Fluid in Overweight Patients with Polycystic Ovary Syndrome. Int. J. Fertil. Steril. 2017, 11, 105–111. [Google Scholar] [CrossRef]
- Zhao, J.; Liu, S.; Wang, Y.; Wang, P.; Qu, D.; Liu, M.; Ma, W.; Li, Y. Vitamin D improves in-vitro fertilization outcomes in infertile women with polycystic ovary syndrome and insulin resistance. Minerva Med. 2019, 110, 199–208. [Google Scholar] [CrossRef]
- Chakraborty, P.; Goswami, S.K.; Rajani, S.; Sharma, S.; Kabir, S.N.; Chakravarty, B.; Jana, K. Recurrent Pregnancy Loss in Polycystic Ovary Syndrome: Role of Hyperhomocysteinemia and Insulin Resistance. PLoS ONE 2013, 8, e64446. [Google Scholar] [CrossRef]
- Lerchbaum, E.; Obermayer-Pietsch, B. MECHANISMS IN ENDOCRINOLOGY: Vitamin D and fertility: A systematic review. Eur. J. Endocrinol. 2012, 166, 765–778. [Google Scholar] [CrossRef]
- van der Spuy, Z.M.; Dyer, S.J. The pathogenesis of infertility and early pregnancy loss in polycystic ovary syndrome. Best Pract. Res. Clin. Obs. Gynaecol. 2004, 18, 755–771. [Google Scholar] [CrossRef]
- Pittas, A.G.; Lau, J.; Hu, F.B.; Dawson-Hughes, B. The Role of Vitamin D and Calcium in Type 2 Diabetes. A Systematic Review and Meta-Analysis. J. Clin. Endocrinol. Metab. 2007, 92, 2017–2029. [Google Scholar] [CrossRef]
- Shahrokhi, S.Z.; Ghaffari, F.; Kazerouni, F. Role of vitamin D in female Reproduction. Clin. Chim. Acta 2016, 455, 33–38. [Google Scholar] [CrossRef]
- Hahn, S.; Haselhorst, U.; Tan, S.; Quadbeck, B.; Schmidt, M.; Roesler, S.; Kimmig, R.; Mann, K.; Janssen, O.E. Low Serum 25-Hydroxyvitamin D Concentrations are Associated with Insulin Resistance and Obesity in Women with Polycystic Ovary Syndrome. Exp. Clin. Endocrinol. Diabetes 2006, 114, 577–583. [Google Scholar] [CrossRef]
- Pittas, A.G.; Harris, S.S.; Stark, P.C.; Dawson-Hughes, B. The effects of calcium and vitamin D supplementation on blood glucose and markers of inflammation in nondiabetic adults. Diabetes Care 2007, 30, 980–986. [Google Scholar] [CrossRef] [Green Version]
- Yates, N.; Crew, R.C.; Wyrwoll, C.S. Vitamin D deficiency and impaired placental function: Potential regulation by glucocorticoids? Reproduction 2017, 153, R163–R171. [Google Scholar] [CrossRef] [Green Version]
- Tavakoli, M.; Jeddi-Tehrani, M.; Salek-Moghaddam, A.; Rajaei, S.; Mohammadzadeh, A.; Sheikhhasani, S.; Kazemi-Sefat, G.E.; Zarnani, A.H. Effects of 1,25(OH)2 vitamin D3 on cytokine production by endometrial cells of women with recurrent spontaneous abortion. Fertil. Steril. 2011, 96, 751–757. [Google Scholar] [CrossRef]
- Díaz, L.; Noyola-Martínez, N.; Barrera, D.; Hernández, G.; Avila, E.; Halhali, A.; Larrea, F. Calcitriol inhibits TNF-α-induced inflammatory cytokines in human trophoblasts. J. Reprod. Immunol. 2009, 81, 17–24. [Google Scholar] [CrossRef]
- Liu, N.; Kaplan, A.; Low, J.; Nguyen, L.; Liu, G.; Equils, O.; Hewison, M. Vitamin D Induces Innate Antibacterial Responses in Human Trophoblasts via an Intracrine Pathway1. Biol. Reprod. 2009, 80, 398–406. [Google Scholar] [CrossRef] [Green Version]
- Lee, C.L.; Ng, B.K.; Wu, L.L.; Cheah, F.C.; Othman, H.; Ismail, N.A.M. Vitamin D deficiency in pregnancy at term: Risk factors and pregnancy outcomes. Horm. Mol. Biol. Clin. Investig. 2017, 3, 31. [Google Scholar] [CrossRef]
- Knabl, J.; Vattai, A.; Ye, Y.; Jueckstock, J.; Hutter, S.; Kainer, F.; Mahner, S.; Jeschke, U. Role of Placental VDR Expression and Function in Common Late Pregnancy Disorders. Int. J. Mol. Sci. 2017, 18, 2340. [Google Scholar] [CrossRef] [Green Version]
- Xu, C.; Ma, H.H.; Wang, Y. Maternal Early Pregnancy Plasma Concentration of 25-Hydroxyvitamin D and Risk of Gestational Diabetes Mellitus. Calcif. Tissue Res. 2018, 102, 280–286. [Google Scholar] [CrossRef]
- Zhang, M.X.; Pan, G.T.; Guo, J.F.; Li, B.Y.; Qin, L.Q.; Zhang, Z.L. Vitamin D Deficiency Increases the Risk of Gestational Diabetes Mellitus: A Meta-Analysis of Observational Studies. Nutrients 2015, 7, 8366–8375. [Google Scholar] [CrossRef] [Green Version]
- Grundmann, M.; von Versen-Hoynck, F. Vitamin D-roles in women’s reproductive health? Reprod. Biol. Endocrinol. 2011, 9, 146. [Google Scholar] [CrossRef] [Green Version]
- Xiaomang, J.; Yanling, W. Effect of vitamin D3 supplementation during pregnancy on high risk factors—A randomized controlled trial. J. Périnat. Med. 2021, 49, 480–484. [Google Scholar] [CrossRef]
- Rahnemaei, F.A.; Fashami, M.A.; Abdi, F.; Abbasi, M. Factors effective in the prevention of Preeclampsia: A systematic review. Taiwan J. Obstet. Gynecol. 2020, 59, 173–182. [Google Scholar] [CrossRef]
- Stougaard, M.; Damm, P.; Frederiksen, P.; Jacobsen, R.; Heitmann, B.L. Extra vitamin D from fortification and the risk of preeclampsia: The D-tect Study. PLoS ONE 2018, 13, e0191288. [Google Scholar] [CrossRef] [Green Version]
- Schulz, E.V.; Cruze, L.; Wei, W.; Gehris, J.; Wagner, C.L. Maternal vitamin D sufficiency and reduced placental gene expression in angiogenic biomarkers related to comorbidities of pregnancy. J. Steroid Biochem. Mol. Biol. 2017, 173, 273–279. [Google Scholar] [CrossRef]
- Zhang, J.Y.; Wu, P.; Chen, D.; Ning, F.; Lu, Q.; Qiu, X.; Hewison, M.; Tamblyn, J.A.; Kilby, M.D.; Lash, G.E. Vitamin D Promotes Trophoblast Cell Induced Separation of Vascular Smooth Muscle Cells in Vascular Remodeling via Induction of G-CSF. Front. Cell Dev. Biol. 2020, 8, 601043. [Google Scholar] [CrossRef]
- Hou, H.; Zhang, J.; Chen, D.; Deng, F.; Morse, A.; Qiu, X.; He, P.; Lash, G. Altered decidual and placental catabolism of vitamin D may contribute to the aetiology of spontaneous miscarriage. Placenta 2020, 92, 1–8. [Google Scholar] [CrossRef]
- Gorelova, I.V.; Popova, P.V.; Rulev, M.V. Vitamin D and reproductive health. Probl. Endokrinol. Mosk 2020, 66, 96–101. [Google Scholar] [CrossRef]
- Bubanovic, I. 1α,25-dihydroxy-vitamin-D3 as new immunotherapy in treatment of recurrent spontaneous abortion. Med. Hypotheses 2004, 63, 250–253. [Google Scholar] [CrossRef]
- Andersen, L.B.; Jorgensen, J.S.; Jensen, T.K.; Dalgård, C.; Barington, T.; Nielsen, J.; Beck-Nielsen, S.S.; Husby, S.; Abrahamsen, B.; Lamont, R.F.; et al. Vitamin D insufficiency is associated with increased risk of first-trimester miscarriage in the Odense Child Cohort. Am. J. Clin. Nutr. 2015, 102, 633–638. [Google Scholar] [CrossRef] [Green Version]
- Jefferson, K.K.; Parikh, H.; Garcia, E.M.; Edwards, D.J.; Serrano, M.G.; Hewison, M.; Shary, J.R.; Powell, A.M.; Hollis, B.W.; Fettweis, J.M.; et al. Relationship between vitamin D status and the vaginal microbiome during pregnancy. J. Perinatol. 2019, 39, 824–836. [Google Scholar] [CrossRef]
- Wagner, C.L.; Hollis, B.W. Early-Life Effects of Vitamin D: A Focus on Pregnancy and Lactation. Ann. Nutr. Metab. 2020, 76, 16–28. [Google Scholar] [CrossRef]
- McDonnell, S.L.; Baggerly, K.A.; Baggerly, C.A.; Aliano, J.L.; French, C.B.; Baggerly, L.L.; Ebeling, M.D.; Rittenberg, C.S.; Goodier, C.G.; Mateus Niño, J.F.; et al. Maternal 25(OH)D concentrations >/=40 ng/mL associated with 60% lower preterm birth risk among general obstetrical patients at an urban medical center. PLoS ONE 2017, 12, e0180483. [Google Scholar] [CrossRef] [Green Version]
- Uçar, N.; Grant, W.B.; Peraita-Costa, I.; Suárez-Varela, M.M. How 25(OH)D Levels during Pregnancy Affect Prevalence of Autism in Children: Systematic Review. Nutrients 2020, 12, 2311. [Google Scholar] [CrossRef]
- Li, Y.X.; Long, D.L.; Liu, J.; Qiu, D.; Wang, J.; Cheng, X.; Yang, X.; Li, R.M.; Wang, G. Gestational diabetes mellitus in women increased the risk of neonatal infection via inflammation and autophagy in the placenta. Medicine 2020, 99, e22152. [Google Scholar] [CrossRef]
- Zur, R.L.; Kingdom, J.C.; Parks, W.T.; Hobson, S.R. The Placental Basis of Fetal Growth Restriction. Obstet. Gynecol. Clin. N. Am. 2020, 47, 81–98. [Google Scholar] [CrossRef]
- Schoots, M.H.; Gordijn, S.J.; Scherjon, S.A.; van Goor, H.; Hillebrands, J.L. Oxidative stress in placental pathology. Placenta 2018, 69, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.P.H.; Yong, H.E.J.; Chollangi, T.; Borg, A.J.; Brennecke, S.P.; Murthi, P. Placental vitamin D receptor expression is decreased in human idiopathic fetal growth restriction. Klin. Wochenschr. 2015, 93, 795–805. [Google Scholar] [CrossRef] [PubMed]
- Dimasuay, K.G.; Boeuf, P.; Powell, T.L.; Jansson, T. Placental Responses to Changes in the Maternal Environment Determine Fetal Growth. Front. Physiol. 2016, 7, 12. [Google Scholar] [CrossRef] [Green Version]
- Wilson, R.L.; Buckberry, S.; Spronk, F.; Laurence, J.A.; Leemaqz, S.; O’Leary, S.; Bianco-Miotto, T.; Du, J.; Anderson, P.H.; Roberts, C.T. Vitamin D Receptor Gene Ablation in the Conceptus Has Limited Effects on Placental Morphology, Function and Pregnancy Outcome. PLoS ONE 2015, 10, e0131287. [Google Scholar] [CrossRef] [Green Version]
- Cleal, J.K.; Day, P.E.; Simner, C.L.; Barton, S.J.; Mahon, P.A.; Inskip, H.M.; Godfrey, K.M.; Hanson, M.A.; Cooper, C.; Lewis, R.M.; et al. Placental amino acid transport may be regulated by maternal vitamin D and vitamin D-binding protein: Results from the Southampton Women’s Survey. Br. J. Nutr. 2015, 113, 1903–1910. [Google Scholar] [CrossRef] [Green Version]
- Raia-Barjat, T.; Sarkis, C.; Rancon, F.; Thibaudin, L.; Gris, J.C.; Alfaidy, N.; Chauleur, C. Vitamin D deficiency during late pregnancy mediates placenta-associated complications. Sci. Rep. 2021, 11, 20708. [Google Scholar] [CrossRef]
- Brodowski, L.; Burlakov, J.; Myerski, A.C.; Von Kaisenberg, C.S.; Grundmann, M.; Hubel, C.A.; Von Versen-Höynck, F. Vitamin D Prevents Endothelial Progenitor Cell Dysfunction Induced by Sera from Women with Preeclampsia or Conditioned Media from Hypoxic Placenta. PLoS ONE 2014, 9, e98527. [Google Scholar] [CrossRef] [Green Version]
- Javorski, N.; Lima, C.; Silva, L.; Crovella, S.; Silva, J.D.A. Vitamin D receptor (VDR) polymorphisms are associated to spontaneous preterm birth and maternal aspects. Gene 2018, 642, 58–63. [Google Scholar] [CrossRef]
- Wang, B.; Ithier, M.C.; Parobchak, N.; Yadava, S.M.; Schulkin, J.; Rosen, T. Vitamin D stimulates multiple microRNAs to inhibit CRH and other pro-labor genes in human placenta. Endocr. Connect. 2018, 7, 1380–1388. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Wang, T.; Huo, Y.; Liu, L.; Liu, S.; Yin, X.; Wang, R.; Gao, X. Placenta expression of vitamin D and related genes in pregnant women with gestational diabetes mellitus. J. Steroid Biochem. Mol. Biol. 2020, 204, 105754. [Google Scholar] [CrossRef]
- Knabl, J.; Hüttenbrenner, R.; Hutter, S.; Günthner-Biller, M.; Riedel, C.; Hiden, U.; Kainer, F.; Desoye, G.; Jeschke, U. Gestational Diabetes Mellitus Upregulates Vitamin D Receptor in Extravillous Trophoblasts and Fetoplacental Endothelial Cells. Reprod. Sci. 2015, 22, 358–366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lacroix, M.; Lizotte, F.; Hivert, M.F.; Geraldes, P.; Perron, P. Calcifediol Decreases Interleukin-6 Secretion by Cultured Human Trophoblasts from GDM Pregnancies. J. Endocr. Soc. 2019, 3, 2165–2178. [Google Scholar] [CrossRef] [PubMed]
- Tan, M.L.; Abrams, S.A.; Osborn, D.A. Vitamin D supplementation for term breastfed infants to prevent vitamin D deficiency and improve bone health. Cochrane Database Syst. Rev. 2018, 83, 013046. [Google Scholar] [CrossRef]
- Wang, C.; Gao, J.; Liu, N.; Yu, S.; Qiu, L.; Wang, D. Maternal factors associated with neonatal vitamin D deficiency. J. Pediatr. Endocrinol. Metab. 2019, 32, 167–172. [Google Scholar] [CrossRef]
- Merewood, A.; Mehta, S.D.; Chen, T.C.; Bauchner, H.; Holick, M.F. Association between Vitamin D Deficiency and Primary Cesarean Section. J. Clin. Endocrinol. Metab. 2009, 94, 940–945. [Google Scholar] [CrossRef] [Green Version]
- Maugeri, A.; Barchitta, M.; Blanco, I.; Agodi, A. Effects of Vitamin D Supplementation During Pregnancy on Birth Size: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients 2019, 11, 442. [Google Scholar] [CrossRef] [Green Version]
- Brooke, O.G.; Brown, I.R.; Bone, C.D.; Carter, N.D.; Cleeve, H.J.; Maxwell, J.D.; Robinson, V.P.; Winder, S.M. Vitamin D supplements in pregnant Asian women: Effects on calcium status and fetal growth. BMJ 1980, 280, 751–754. [Google Scholar] [CrossRef] [Green Version]
- Dror, D.K. Vitamin D status during pregnancy: Maternal, fetal, and postnatal outcomes. Curr. Opin. Obstet. Gynecol. 2011, 23, 422–426. [Google Scholar] [CrossRef]
- Pasco, J.A.; Wark, J.D.; Carlin, J.B.; Ponsonby, A.L.; Vuillermin, P.J.; Morley, R. Maternal vitamin D in pregnancy may influence not only offspring bone mass but other aspects of musculoskeletal health and adiposity. Med. Hypotheses 2008, 71, 266–269. [Google Scholar] [CrossRef]
- Cranney, A.; Horsley, T.; O’Donnell, S.; Weiler, H.; Puil, L.; Ooi, D.; Atkinson, S.; Ward, L.; Moher, D.; Hanley, D.; et al. Effectiveness and safety of vitamin D in relation to bone health. Évid. Rep. Technol. Assess. 2007, 158, 1–235. [Google Scholar]
- Møller, U.K.; Streym, S.V.; Mosekilde, L.; Rejnmark, L. Changes in bone mineral density and body composition during pregnancy and postpartum. A controlled cohort study. Osteoporos. Int. 2012, 23, 1213–1223. [Google Scholar] [CrossRef] [PubMed]
- Breasail, M.Ó.; Prentice, A.; Ward, K. Pregnancy-Related Bone Mineral and Microarchitecture Changes in Women Aged 30 to 45 Years. J. Bone Miner. Res. 2020, 35, 1253–1262. [Google Scholar] [CrossRef] [PubMed]
- Curtis, E.M.; Parsons, C.; Maslin, K.; D’Angelo, S.; Moon, R.J.; Crozier, S.R.; Gossiel, F.; Bishop, N.J.; Kennedy, S.H.; Papageorghiou, A.T.; et al. Bone turnover in pregnancy, measured by urinary CTX, is influenced by vitamin D supplementation and is associated with maternal bone health: Findings from the Maternal Vitamin D Osteoporosis Study (MAVIDOS) trial. Am. J. Clin. Nutr. 2021, 114, 1600–1611. [Google Scholar] [CrossRef] [PubMed]
- Pludowski, P.; Grant, W.; Bhattoa, H.P.; Bayer, M.; Povoroznyuk, V.; Rudenka, E.; Ramanau, H.; Varbiro, S.; Rudenka, A.; Karczmarewicz, E.; et al. Vitamin D Status in Central Europe. Int. J. Endocrinol. 2014, 2014, 589587. [Google Scholar] [CrossRef]
- Pludowski, P.; Holick, M.F.; Grant, W.B.; Konstantynowicz, J.; Mascarenhas, M.R.; Haq, A.; Povoroznyuk, V.; Balatska, N.; Barbosa, A.P.; Karonova, T.; et al. Vitamin D supplementation guidelines. J. Steroid Biochem. Mol. Biol. 2018, 175, 125–135. [Google Scholar] [CrossRef] [Green Version]
- Płudowski, P.; Karczmarewicz, E.; Bayer, M.; Carter, G.; Chlebna-Sokół, D.; Czech-Kowalska, J.; Dębski, R.; Decsi, T.; Dobrzańska, A.; Franek, E.; et al. Practical guidelines for the supplementation of vitamin D and the treatment of deficits in Central Europe—Recommended vitamin D intakes in the general population and groups at risk of vitamin D deficiency. Endokrynol. Polska 2013, 64, 319–327. [Google Scholar] [CrossRef]
- Takács, I.; Benkő, I.; Toldy, E.; Wikonkál, N.; Szekeres, L.; Bodolay, E.; Kiss, E.; Jambrik, Z.; Szabó, B.; Merkely, B.; et al. Hungarian consensus regarding the role of vitamin D in the prevention and treatment of diseases. Orv. Hetil. 2012, 153, 5–26. [Google Scholar] [CrossRef] [Green Version]
- Quaresima, P.; Angeletti, M.; Luziatelli, D.; Luziatelli, S.; Venturella, R.; Di Carlo, C.; Bernardo, S. Pregnancy associated transient osteoporosis of the hip (PR-TOH): A non–obstetric indication to caesarean section. A case report with literature review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 262, 28–35. [Google Scholar] [CrossRef]
- teib-Furno, S.; Mathieu, L.; Pham, T.; Armingeat, T.; Porcu, G.; Gamerre, M.; Chagnaud, C.; Lafforgue, P. Pregnancy-related hip diseases: Incidence and diagnoses. Jt. Bone Spine 2007, 74, 373–378. [Google Scholar] [CrossRef]
- Bouillon, R.; Marcocci, C.; Carmeliet, G.; Bikle, D.; White, J.H.; Dawson-Hughes, B.; Lips, P.; Munns, C.F.; Lazaretti-Castro, M.; Giustina, A.; et al. Skeletal and Extraskeletal Actions of Vitamin D: Current Evidence and Outstanding Questions. Endocr. Rev. 2019, 40, 1109–1151. [Google Scholar] [CrossRef] [Green Version]
- Hu, K.L.; Zhang, C.X.; Chen, P.; Zhang, D.; Hunt, S. Vitamin D Levels in Early and Middle Pregnancy and Preeclampsia, a Systematic Review and Meta-Analysis. Nutrients 2022, 14, 999. [Google Scholar] [CrossRef]
- Wierzejska, R. Evaluation of prenatal vitamin-mineral preparations in the context of recommended dietary supplementation. Are pregnant women supplied with what they should get? Rocz. Państwowego Zakładu Hig. 2021, 72, 309–320. [Google Scholar] [CrossRef]
- Wierzejska, R.E. Review of Dietary Recommendations for Twin Pregnancy: Does Nutrition Science Keep Up with the Growing Incidence of Multiple Gestations? Nutrients 2022, 14, 1143. [Google Scholar] [CrossRef]
- Takács, I.; Benkő, I.; Toldy, E.; Wikonkál, N.; Szekeres, L.; Bodolay, E.; Kiss, E.; Jambrik, Z.; Szabó, B.; Merkely, B.; et al. Harmadik magyarországi konszenzus a D-vitamin szerepéről a betegségek megelőzésében és kezelésében. Orv. Szle. 2016, 2, 13–26. [Google Scholar]
- Kimball, S.M.; Holick, M.F. Official recommendations for vitamin D through the life stages in developed countries. Eur. J. Clin. Nutr. 2020, 74, 1514–1518. [Google Scholar] [CrossRef]
- Pludowski, P.; Takacs, I.; Boyanov, M.; Belaya, Z.; Diaconu, C.C.; Mokhort, T.; Zherdova, N.; Rasa, I.; Payer, J.; Pilz, S. Clinical Practice in the Prevention, Diagnosis and Treatment of Vitamin D Deficiency: A Central and Eastern European Expert Consensus Statement. Nutrients 2022, 14, 1483. [Google Scholar] [CrossRef]
- Lemke, D.; Klement, R.J.; Schweiger, F.; Schweiger, B.; Spitz, J. Vitamin D Resistance as a Possible Cause of Autoimmune Diseases: A Hypothesis Confirmed by a Therapeutic High-Dose Vitamin D Protocol. Front. Immunol. 2021, 12, 655739. [Google Scholar] [CrossRef]
| Study | Article Type | Study Group | Summary |
| Xu et al. [25] | Cell line (animal) | Secondary preantral follicles were isolated from ovaries of rhesus monkeys | Vitamin D increases survival of the preantral follicle, sustains AMH production and enhances the growth of the antral follicle. |
| Kinute et al. [21] | Animal Study | VDR null mutant mice (n = 3–10 group) | In females: uterine hypoplasia, decreased aromatase activity and aromatase gene expression were observed; in males: decreased sperm count and decreased motility with histological abnormality of the testis were observed. |
| Akhavizadegan et al. [22] | Case control study | Fertile men (n = 116) and infertile men (n = 114) | Men with vitamin D levels below 20 ng/mL have significantly lower sperm counts. The mean vitamin D level in the fertile group was significantly higher than in the infertile group. |
| Dennis et al. [19] | Correlative and intervention study | Mature men (n = 113), premenopausal women (n = 35), 5- to 6-yr-old boys (n = 74) | Serum AMH correlates positively with vitamin D levels in men (but not in boys). Vitamin D levels and AMH levels show a seasonal difference in women, with AMH levels falling by 18% in the winter compared to summer. The change in AMH levels correlates with initial AMH levels and the magnitude of the change in vitamin D levels. Vitamin D supplementation prevents seasonal AMH change. |
| Ozkan et al. [24] | Prospective Cohort Study | Infertile women undergoing IVF (n = 84) | Vitamin D level influences the outcomes of IVF independently of age, BMI, ethnicity and the number of embryo transfers. Vitamin D levels correlate strongly (r = 0.94) with follicular fluid. |
| Study | Article Type | Study Group | Summary |
| Tavakoli et al. [48] | Cell line (human) | Endometrial samples (from women with recurrent spontaneous abortion and healthy controls) | Vitamin D supplementation may have a beneficial effect in case of recurrent miscarriages. As a result of vitamin D supplementation, Th2 cytokine dominance was observed with decreased proliferation of inflammatory cytokines. |
| Diaz et al. [49] | Cell line (human) | Term placentae samples (37–41 weeks of gestation, from uncomplicated pregnancies) | Calcitriol supplementation prevents the production of TNF alpha, IL-6 and IFN gamma—this is likely mediated by VDR. |
| Liu et al. [50] | Cell line (human) | Human trophoblastic cell lines from American Type Tissue Culture Collection | In human trophoblast cells, Vitamin D metabolites significantly enhance antibacterial responses. |
| Kuyucu et al. [34] | Animal study | Prepubertal female rats, control group (n = 8), PCOS group (n = 8) and PCOS + D3 group (n = 8) | Vitamin D treatment significantly reduced endometrial, epithelial and stromal thickness in PCOS patients, as well as pathological proliferation and apoptosis. AMH was also decreased as a result of vitamin D supplementation (this however did not reach the level of significance). |
| Guo et al. [36] | Case control study | Endometrial samples from women who underwent standardized IVF treatment (n = 16) | VDR plays role in the development of endometrial susceptibility: increased VDR expression in the endometrium (especially in the implantation window of the menstrual cycle) is significantly more likely to lead to pregnancy. |
| Zadeh-Vakili et al. [32] | Case control study | PCOS women (n = 260) and women with physiological cycles (n = 221) | The genetic variant of VDR is associated with the severity of the clinical features of PCOS, but not with the risk of the disease itself. |
| Aghadavod et al. [38] | Case control study | Control group (n = 20 normal weights and n = 20 over-weights); PCOS group (n = 20 normal weight and n = 20 over-weight) | Vitamin D levels in follicular fluid are significantly lower in PCOS and overweight patients. Vitamin D levels in follicular fluid strongly correlate with BMI. VDR expression in granulosa cells is significantly lower in PCOS/overweight patients than in non PCOS or normal weight individuals. |
| Zhao et al. [39] | Case control study | In total, 305 women were divided into 4 groups based on serum vitamin D levels. | Optimal vitamin D levels improve embryo quality and lead to significantly higher clinical pregnancy rates. |
| March et al. [27] | Retrospective birth cohort study | In total, 728 women born between 1973–1975 in a single maternity hospital were traced and interviewed in adulthood (age = 27–34 year; n = 728). | Prevalence estimates for Rotterdam and AES may be up two twice of that for NIH criteria A significant proportion of women with PCOS are not diagnosed or are diagnosed late. |
| Pal et al. [28] | Retrospective cohort study (Secondary analysis of randomized controlled trial data) | Participants in the Pregnancy in PCOS I randomized controlled trial (n = 540) who met the National Institutes of Health diagnostic criteria for PCOS. | In women with PCOS, serum vitamin D level is an independent predictor of reproductive success rates following induction of ovulation. Probability of ovulation correlates with vitamin D levels in PCOS. The reproductive threshold for serum vitamin D is higher in than that recommended for the non-pregnant population. |
| Hahn et al. [45] | Prospective cohort study | PCOS women (n = 120) | In PCOS, insulin resistance correlates negatively with vitamin D levels. |
| Pittas et al. [46] | Randomized controlled trial | Caucasian adults (n = 314) | In older healthy adults with impaired fasting glucose (IFG), calcium and vitamin D supplementation may reduce the further development of insulin resistance. |
| Study | Article Type | Study Group | Summary |
|---|---|---|---|
| Wilson et al. [74] | Animal study | VDR+/− virgin female mice (n = 12) + VDR+/− male mice | In VDR−/− placenta, the expression of Deptor and Prr5 involved in mTOR signaling was decreased significantly. |
| Cleal et al. [75] | Cell line (human) | Placental samples collected in the Southampton Women’s Survey (n = 102) | Maternal vitamin D and vitamin-D-binding protein levels correlate positively with the expression of amino-acid transporter genes of the placenta. |
| Brodowski et al. [77] | Cell line (human) | Cord blood samples from uncomplicated pregnancies and uncomplicated pregnancy villous placentae | Vitamin D promotes the formation of capillary-like tubules and the migration of endothelial colony-forming cells, minimizing the negative effects of preeclampsia. |
| Wang et al. [79] | Cell line (human) | Placenta samples from healthy women (38–40 weeks of gestations) | Vitamin D downregulates pro-labor genes such as corticotropin-releasing hormone. This reduces the risk of preterm birth. |
| Javorski et al. [78] | Cell line (human) | Pregnant women (n = 189) | Polymorphisms in the VDR gene (Fok-l and Cdx-2) increase the risk of spontaneous preterm birth. |
| Wang et al. [80] | Case-control study | GDM women (n = 41) and healthy pregnant women (n = 40) | Placental CYP24A1 protein and mRNA levels responsible for vitamin D catabolism, VDR protein and mRNA levels are increased in GDM. |
| Knabl et al. [81] | Case-control study | Placental tissue samples from GDM and control patients (n = 40 GDM and n = 40 controls) | VDR expression is regulated in a bimodal fashion by calcitriol: high doses (0.1 and 1 nmol/mL) lead to downregulation, while low doses (0.01 nmol/mL) lead to VDR upregulation. |
| Lacroix et al. [82] | Case-control study | Placental tissue samples from normoglycemic and GDM women. | VDR protein expression was increased in GDM patient placenta samples; Vitamin D decreases IL-6 secretion. |
| Hou et al. [61] | Case-control study | Placenta and decidua samples were collected following termination of pregnancy (controls n = 20 and spontaneous miscarriage n = 20) | In cases of spontaneous miscarriage, placental and decidual expression of both the vitamin D receptor and the vitamin-D-binding protein was increased. Women who undergo assisted reproductive technologies should ensure optimal vitamin D levels prior to pregnancy. |
| Nguyen et al. [72] | Case-control study | Placentae from pregnancies complicated by idiopathic fetal growth restriction (n = 25) and gestational-matched controls (n = 25) | In cases of idiopathic fetal growth restriction, VDR mRNA and protein levels were all significantly decreased. |
| Stougaard et al. [58] | Retrospective cohort study | Woman who gave birth between 1983–1988 (n = 73,237) | There is no association between increased dietary intake of vitamin D and the incidence of preeclampsia. |
| Merewood et al. [85] | Retrospective cohort study | Women (n = 253) who had undergone a primary cesarean section (n = 43) | There is a negative association between maternal serum vitamin D levels and cesarean sections. Women with vitamin D levels below 37.5 nmol/L were almost four times more likely to have a cesarean section. |
| Lee et al. [51] | Prospective observational study | Women who completed 37 weeks of pregnancy (n = 680) | In total, 71.7% of pregnant women were vitamin D deficient, 21.0% of pregnant women were vitamin D insufficient and 7.3% of pregnant women had adequate vitamin D levels. |
| Xu et al. [53] | Prospective cohort study | Pregnant women (n = 827, 101 developed GDM) | Median plasma vitamin D concentrations at the first prenatal visit were significantly lower in women who later developed GMD. |
| Andersen et al. [64] | Prospective cohort study | Pregnant women (n = 1683) | The adjusted hazard of first trimester miscarriage is lower at higher vitamin D levels: vitamin D levels below 50 ng/mL double the risk of a miscarriage. No such relationship was found in the second trimester. |
| McDonnell et al. [67] | Prospective cohort study | Pregnant women (n = 1064) | Maternal vitamin D levels above 40 ng/mL reduce the risk of preterm birth. |
| Raia-Barjat et al. [76] | Prospective multicenter cohort study | Pregnant women (n = 200) | At 32 weeks of gestation, placenta-mediated complications (PMC) were 5-fold higher in vitamin D deficiency patients compared to those with normal vitamin D levels. There is a strong inverse relationship between serum vitamin D levels and the risk of late PMC. Vitamin D plays a role in maintaining placental performance, thus preventing the development of late PMC. |
| Wang et al. [84] | Prospective case-control study | Mother-infant dyads (36.8 ± 2.7 weeks of gestational, n = 125) | In total, 56% of newborns were vitamin D deficient. Neonatal vitamin D deficiency may be associated with winter birth, insufficient sunbathing time, high maternal BMI, insufficient egg consumption, insufficient vitamin D supplementation and adverse health insurance status. |
| Xiaomang et al. [56] | Randomized controlled trial | Women who had undergone maternity treatment and delivery (n = 450) | Vitamin D supplementation may reduce the incidence of preeclampsia while also lowering the IUGR index. |
| Schulz et al. [59] | Randomized controlled trial | Pregnant women (n = 43) | Serum vitamin D levels above 100 ng/mL reduce the expression of soluble Fms-like tyrosine kinase-1 (sFlt-1) and VEGF. Maternal vitamin D supplementation may reduce the transcription of genes that contribute to preeclampsia. |
| Jefferson et al. [65] | Randomized controlled trial | Pregnant women (n = 316) | Vitamin D may have a positive impact on the vaginal microbiome: megasphere correlated negatively and L. crispatus correlated positively with plasma vitamin D levels. |
| Brooke et al. [87] | Randomized controlled trial | Pregnant women (D-vitamin treated n = 59 and control n = 67) during the last trimester | The risk of SGA in the control group was almost twice that found in the vitamin-D-supplemented group. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Várbíró, S.; Takács, I.; Tűű, L.; Nas, K.; Sziva, R.E.; Hetthéssy, J.R.; Török, M. Effects of Vitamin D on Fertility, Pregnancy and Polycystic Ovary Syndrome—A Review. Nutrients 2022, 14, 1649. https://doi.org/10.3390/nu14081649
Várbíró S, Takács I, Tűű L, Nas K, Sziva RE, Hetthéssy JR, Török M. Effects of Vitamin D on Fertility, Pregnancy and Polycystic Ovary Syndrome—A Review. Nutrients. 2022; 14(8):1649. https://doi.org/10.3390/nu14081649
Chicago/Turabian StyleVárbíró, Szabolcs, István Takács, László Tűű, Katalin Nas, Réka Eszter Sziva, Judit Réka Hetthéssy, and Marianna Török. 2022. "Effects of Vitamin D on Fertility, Pregnancy and Polycystic Ovary Syndrome—A Review" Nutrients 14, no. 8: 1649. https://doi.org/10.3390/nu14081649
APA StyleVárbíró, S., Takács, I., Tűű, L., Nas, K., Sziva, R. E., Hetthéssy, J. R., & Török, M. (2022). Effects of Vitamin D on Fertility, Pregnancy and Polycystic Ovary Syndrome—A Review. Nutrients, 14(8), 1649. https://doi.org/10.3390/nu14081649