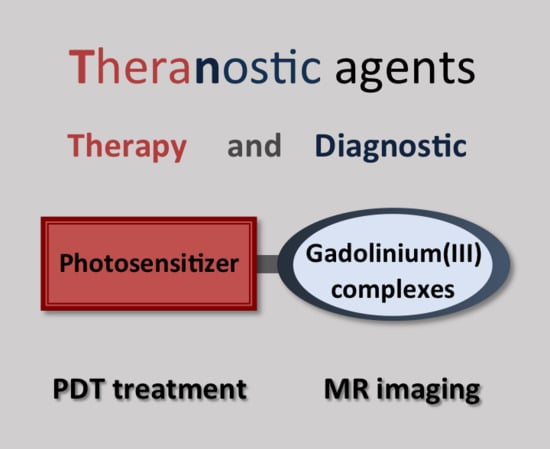
Molecular Theranostic Agents for Photodynamic Therapy (PDT) and Magnetic Resonance Imaging (MRI)
Abstract
:1. Introduction to the Theranostic Approach
1.1. PDT Treatment: Strengths and Limitations
1.2. MRI Guidance of PDT
2. Porphyrin-Gd-Complexes Conjugates with Potential MRI and PDT Applications
3. Molecular Theranostic Agents with Combined PDT and MRI Studies
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Yoon, H.Y.; Jeon, S.; You, D.G.; Park, J.H.; Kwon, I.C.; Koo, H.; Kim, K. Inorganic Nanoparticles for Image-Guided Therapy. Bioconj. Chem. 2017, 28, 124–134. [Google Scholar] [CrossRef] [PubMed]
- Crawley, N.; Thompson, M.; Romaschin, A. Theranostics in the Growing Field of Personalized Medicine: An Analytical Chemistry Perspective. Anal. Chem. 2014, 86, 130–160. [Google Scholar] [CrossRef] [PubMed]
- Terreno, E.; Uggeri, F.; Aime, S. Image guided therapy: The advent of theranostic agents. J. Control. Release 2012, 161, 328–337. [Google Scholar] [CrossRef] [PubMed]
- Kelkar, S.S.; Reineke, T.M. Theranostics: Combining Imaging and Therapy. Bioconj. Chem. 2011, 22, 1879–1903. [Google Scholar] [CrossRef] [PubMed]
- Kunjachan, S.; Ehling, J.; Storm, G.; Kiessling, F.; Lammers, T. Noninvasive Imaging of Nanomedicines and Nanotheranostics: Principles, Progress, and Prospects. Chem. Rev. 2015, 115, 10907–10937. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Roy, I.; Yang, C.; Prasad, P.N. Nanochemistry and Nanomedicine for Nanoparticle-based Diagnostics and Therapy. Chem. Rev. 2016, 116, 2826–2885. [Google Scholar] [CrossRef] [PubMed]
- Björnmalm, M.; Thurecht, K.J.; Michael, M.; Scott, A.M.; Caruso, F. Bridging Bio–Nano Science and Cancer Nanomedicine. ACS Nano 2017, 11, 9594–9613. [Google Scholar] [CrossRef]
- Fan, W.; Huang, P.; Chen, X. Overcoming the Achilles’ heel of photodynamic therapy. Chem. Soc. Rev. 2016, 45, 6488–6519. [Google Scholar] [CrossRef]
- Abrahamse, H.; Hamblin, M.R. New photosensitizers for photodynamic therapy. Biochem. J. 2016, 473, 347–364. [Google Scholar] [CrossRef] [Green Version]
- Dąbrowski, J.M.; Arnaut, L.G. Photodynamic therapy (PDT) of cancer: From local to systemic treatment. Photochem. Photobiol. Sci. 2015, 14, 1765–1780. [Google Scholar] [CrossRef]
- Mroz, P.; Yaroslavsky, A.; Kharkwal, G.B.; Hamblin, M.R. Cell Death Pathways in Photodynamic Therapy of Cancer. Cancers 2011, 3, 2516–2539. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azzouzi, A.-R.; Vincendeau, S.; Barret, E.; Cicco, A.; Kleinclauss, F.; van der Poel, H.G.; Stief, C.G.; Rassweiler, J.; Salomon, G.; Solsona, E.; et al. Padeliporfin vascular-targeted photodynamic therapy versus active surveillance in men with low-risk prostate cancer (CLIN1001 PCM301): An open-label, phase 3, randomised controlled trial. Lancet Oncol. 2017, 18, 181–191. [Google Scholar] [CrossRef]
- Van Straten, D.; Mashayekhi, V.; de Bruijn, H.; Oliveira, S.; Robinson, D. Oncologic Photodynamic Therapy: Basic Principles, Current Clinical Status and Future Directions. Cancers 2017, 9, 19. [Google Scholar] [CrossRef] [PubMed]
- Luz, A.F.S.; Pucelik, B.; Pereira, M.M.; Dąbrowski, J.M.; Arnaut, L.G. Translating phototherapeutic indices from in vitro to in vivo photodynamic therapy with bacteriochlorins. Lasers Surg. Med. 2018, 50, 451–459. [Google Scholar] [CrossRef] [PubMed]
- Celli, J.P.; Spring, B.Q.; Rizvi, I.; Evans, C.L.; Samkoe, K.S.; Verma, S.; Pogue, B.W.; Hasan, T. Imaging and Photodynamic Therapy: Mechanisms, Monitoring, and Optimization. Chem. Rev. 2010, 110, 2795–2838. [Google Scholar] [CrossRef] [Green Version]
- Rai, P.; Mallidi, S.; Zheng, X.; Rahmanzadeh, R.; Mir, Y.; Elrington, S.; Khurshid, A.; Hasan, T. Development and applications of photo-triggered theranostic agents. Adv. Drug Deliv. Rev. 2010, 62, 1094–1124. [Google Scholar] [CrossRef] [Green Version]
- Bhaumik, J.; Mittal, A.K.; Banerjee, A.; Chisti, Y.; Banerjee, U.C. Applications of phototheranostic nanoagents in photodynamic therapy. Nano Res. 2015, 8, 1373–1394. [Google Scholar] [CrossRef]
- Pierre, V.C.; Allen, M.J.; Caravan, P. Contrast agents for MRI: 30+ years and where are we going? JBIC J. Biol. Inorg. Chem. 2014, 19, 127–131. [Google Scholar] [CrossRef] [Green Version]
- Evelhoch, J.L. In vivo MR in the drug pipeline. J. Magn. Reson. 2018, 292, 117–128. [Google Scholar] [CrossRef]
- De León-Rodríguez, L.M.; Martins, A.F.; Pinho, M.C.; Rofsky, N.M.; Sherry, A.D. Basic MR relaxation mechanisms and contrast agent design: MR Relaxation Mechanisms and Contrast Agents. J. Magn. Reson. Imaging 2015, 42, 545–565. [Google Scholar] [CrossRef]
- Josefsen, L.B.; Boyle, R.W. Unique Diagnostic and Therapeutic Roles of Porphyrins and Phthalocyanines in Photodynamic Therapy, Imaging and Theranostics. Theranostics 2012, 2, 916–966. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kennedy, S.D.; Szczepaniak, L.S.; Gibson, S.L.; Hilf, R.; Foster, T.H.; Bryant, R.G. Quantitative MRI of Gd-DTPA uptake in tumors: Response to photo dynamic therapy. Magn. Reson. Med. 1994, 31, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Haider, M.A.; Davidson, S.R.H.; Kale, A.V.; Weersink, R.A.; Evans, A.J.; Toi, A.; Gertner, M.R.; Bogaards, A.; Wilson, B.C.; Chin, J.L.; et al. Prostate Gland: MR Imaging Appearance after Vascular Targeted Photodynamic Therapy with Palladium-Bacteriopheophorbide. Radiology 2007, 244, 196–204. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Haider, M.A.; Kraft, S.; Chen, Q.; Blanc, D.; Wilson, B.C.; Hetzel, F.W. Magnetic resonance imaging correlated with the histopathological effect of Pd-bacteriopheophorbide (Tookad) photodynamic therapy on the normal canine prostate gland. Lasers Surg. Med. 2006, 38, 672–681. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schreurs, T.J.L.; Hectors, S.J.; Jacobs, I.; Grüll, H.; Nicolay, K.; Strijkers, G.J. Quantitative Multi-Parametric Magnetic Resonance Imaging of Tumor Response to Photodynamic Therapy. PLoS ONE 2016, 11, e0165759. [Google Scholar] [CrossRef] [PubMed]
- Zilberstein, J.; Schreiber, S.; Bloemers, M.C.W.M.; Bendel, P.; Neeman, M.; Schechtman, E.; Kohen, F.; Scherz, A.; Salomon, Y. Antivascular Treatment of Solid Melanoma Tumors with Bacteriochlorophyll-serine-based Photodynamic Therapy. Photochem. Photobiol. 2007, 73, 257–266. [Google Scholar] [CrossRef]
- Schleich, N.; Danhier, F.; Préat, V. Iron oxide-loaded nanotheranostics: Major obstacles to in vivo studies and clinical translation. J. Control. Release 2015, 198, 35–54. [Google Scholar] [CrossRef]
- Kumar, R.; Shin, W.S.; Sunwoo, K.; Kim, W.Y.; Koo, S.; Bhuniya, S.; Kim, J.S. Small conjugate-based theranostic agents: An encouraging approach for cancer therapy. Chem. Soc. Rev. 2015, 44, 6670–6683. [Google Scholar] [CrossRef]
- Hofmann, B.; Bogdanov, A.; Marecos, E.; Ebert, W.; Semmler, W.; Weissleder, R. Mechanism of gadophrin-2 accumulation in tumor necrosis. J. Magn. Reson. Imaging 1999, 9, 336–341. [Google Scholar] [CrossRef] [Green Version]
- Barkhausen, J.Ö.; Ebert, W.; Debatin, J.Ö.F.; Weinmann, H.-J. Imaging of myocardial infarction: Comparison of magnevist and gadophrin-3 in rabbits. J. Am. Coll. Cardiol. 2002, 39, 1392–1398. [Google Scholar] [CrossRef]
- Daldrup-Link, H.; Rudelius, M.; Metz, S.; Piontek, G.; Pichler, B.; Settles, M.; Heinzmann, U.; Schlegel, J.R.; Oostendorp, R.J.; Rummeny, E. Cell tracking with gadophrin-2: A bifunctional contrast agent for MR imaging, optical imaging, and fluorescence microscopy. Eur. J. Nucl. Med. Mol. Imaging 2004, 31. [Google Scholar] [CrossRef] [PubMed]
- Metz, S.; Daldrup-Link, H.E.; Richter, T.; Räth, C.; Ebert, W.; Settles, M.; Rummeny, E.J.; Link, T.M.; Piert, M. Detection and Quantification of Breast Tumor Necrosis with MR Imaging. Acad. Radiol. 2003, 10, 484–490. [Google Scholar] [CrossRef]
- Ni, Y. Metalloporphyrins and Functional Analogues as MRI Contrast Agents. Curr. Med. Imaging Rev. 2008, 4, 96–112. [Google Scholar] [CrossRef]
- Haroon Ur, R.; Umar, M.N.; Khan, K.; Anjum, M.N.; Yaseen, M. Synthesis and relaxivity measurement of porphyrin-based Magnetic Resonance Imaging (MRI) contrast agents. J. Struct. Chem. 2014, 55, 910–915. [Google Scholar] [CrossRef]
- Gros, C.P.; Eggenspiller, A.; Nonat, A.; Barbe, J.-M.; Denat, F. New potential bimodal imaging contrast agents based on DOTA-like and porphyrin macrocycles. Med. Chem. Commun. 2011, 2, 119–125. [Google Scholar] [CrossRef]
- Eggenspiller, A.; Michelin, C.; Desbois, N.; Richard, P.; Barbe, J.-M.; Denat, F.; Licona, C.; Gaiddon, C.; Sayeh, A.; Choquet, P.; et al. Design of Porphyrin-dota-Like Scaffolds as All-in-One Multimodal Heterometallic Complexes for Medical Imaging: Porphyrin-dota-Like Scaffolds for Medical Imaging. Eur. J. Org. Chem. 2013, 2013, 6629–6643. [Google Scholar] [CrossRef]
- Trivedi, E.R.; Ma, Z.; Waters, E.A.; Macrenaris, K.W.; Subramanian, R.; Barrett, A.G.M.; Meade, T.J.; Hoffman, B.M. Synthesis and characterization of a porphyrazine-Gd(III) MRI contrast agent and in vivo imaging of a breast cancer xenograft model: TUMOR IMAGING. Contrast Media Mol. Imaging 2014, 9, 313–322. [Google Scholar] [CrossRef]
- Hindré, F.; Plouzennec, M.L.; de Certaines, J.D.; Foultier, M.T.; Patrice, T.; Simonneaux, G. Tetra-p-aminophenylporphyrin conjugated with Gd-DTPA: Tumor-specific contrast agent for MR imaging. J. Magn. Reson. Imaging 1993, 3, 59–65. [Google Scholar] [CrossRef]
- Li, G.; Slansky, A.; Dobhal, M.P.; Goswami, L.N.; Graham, A.; Chen, Y.; Kanter, P.; Alberico, R.A.; Spernyak, J.; Morgan, J.; et al. Chlorophyll-a Analogues Conjugated with Aminobenzyl-DTPA as Potential Bifunctional Agents for Magnetic Resonance Imaging and Photodynamic Therapy. Bioconj. Chem. 2005, 16, 32–42. [Google Scholar] [CrossRef]
- Pandey, R.K.; Goswami, L.N.; Chen, Y.; Gryshuk, A.; Missert, J.R.; Oseroff, A.; Dougherty, T.J. Nature: A rich source for developing multifunctional agents. tumor-imaging and photodynamic therapy. Lasers Surg. Med. 2006, 38, 445–467. [Google Scholar] [CrossRef]
- Spernyak, J.A.; White, W.H.; Ethirajan, M.; Patel, N.J.; Goswami, L.; Chen, Y.; Turowski, S.; Missert, J.R.; Batt, C.; Mazurchuk, R.; et al. Hexylether Derivative of Pyropheophorbide-a (HPPH) on Conjugating with 3 Gadolinium(III) Aminobenzyldiethylenetriaminepentaacetic Acid Shows Potential for in Vivo Tumor Imaging (MR, Fluorescence) and Photodynamic Therapy. Bioconj. Chem. 2010, 21, 828–835. [Google Scholar] [CrossRef] [PubMed]
- Goswami, L.N.; White, W.H.; Spernyak, J.A.; Ethirajan, M.; Chen, Y.; Missert, J.R.; Morgan, J.; Mazurchuk, R.; Pandey, R.K. Synthesis of Tumor-Avid Photosensitizer−Gd(III)DTPA Conjugates: Impact of the Number of Gadolinium Units in T1/T2 Relaxivity, Intracellular localization, and Photosensitizing Efficacy. Bioconj. Chem. 2010, 21, 816–827. [Google Scholar] [CrossRef]
- Lattuada, L.; Barge, A.; Cravotto, G.; Giovenzana, G.B.; Tei, L. The synthesis and application of polyamino polycarboxylic bifunctional chelating agents. Chem. Soc. Rev. 2011, 40, 3019. [Google Scholar] [CrossRef] [PubMed]
- Aydın Tekdaş, D.; Garifullin, R.; Şentürk, B.; Zorlu, Y.; Gundogdu, U.; Atalar, E.; Tekinay, A.B.; Chernonosov, A.A.; Yerli, Y.; Dumoulin, F.; et al. Design of a Gd-DOTA-Phthalocyanine Conjugate Combining MRI Contrast Imaging and Photosensitization Properties as a Potential Molecular Theranostic. Photochem. Photobiol. 2014, 90, 1376–1386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, Y.; Zong, H.; Trivedi, E.R.; Vesper, B.J.; Waters, E.A.; Barrett, A.G.M.; Radosevich, J.A.; Hoffman, B.M.; Meade, T.J. Synthesis and Characterization of New Porphyrazine-Gd(III) Conjugates as Multimodal MR Contrast Agents. Bioconj. Chem. 2010, 21, 2267–2275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lyon, R.C.; Faustino, P.J.; Cohen, J.S.; Katz, A.; Mornex, F.; Colcher, D.; Baglin, C.; Koenig, S.H.; Hambright, P. Tissue distribution and stability of metalloporphyrin MRI contrast agents. Magn. Reson. Med. 1987, 4, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Furmanski, P.; Longley, C. Metalloporphyrin Enhancement of Magnetic Resonance Imaging of Human Tumor Xenografts in Nude Mice. Cancer Res. 1988, 48, 4604–4610. [Google Scholar]
- Yuzhakova, D.V.; Lermontova, S.A.; Grigoryev, I.S.; Muravieva, M.S.; Gavrina, A.I.; Shirmanova, M.V.; Balalaeva, I.V.; Klapshina, L.G.; Zagaynova, E.V. In vivo multimodal tumor imaging and photodynamic therapy with novel theranostic agents based on the porphyrazine framework-chelated gadolinium (III) cation. Biochim. Biophys. Acta Gen. Subj. 2017, 1861, 3120–3130. [Google Scholar] [CrossRef]
- Wu, B.; Li, X.-Q.; Huang, T.; Lu, S.-T.; Wan, B.; Liao, R.-F.; Li, Y.-S.; Baidya, A.; Long, Q.-Y.; Xu, H.-B. MRI-guided tumor chemo-photodynamic therapy with Gd/Pt bifunctionalized porphyrin. Biomater. Sci. 2017, 5, 1746–1750. [Google Scholar] [CrossRef]
- Luo, J.; Chen, L.-F.; Hu, P.; Chen, Z.-N. Tetranuclear Gadolinium(III) Porphyrin Complex as a Theranostic Agent for Multimodal Imaging and Photodynamic Therapy. Inorg. Chem. 2014, 53, 4184–4191. [Google Scholar] [CrossRef]
- Sour, A.; Jenni, S.; Ortí-Suárez, A.; Schmitt, J.; Heitz, V.; Bolze, F.; Loureiro de Sousa, P.; Po, C.; Bonnet, C.S.; Pallier, A.; et al. Four Gadolinium(III) Complexes Appended to a Porphyrin: A Water-Soluble Molecular Theranostic Agent with Remarkable Relaxivity Suited for MRI Tracking of the Photosensitizer. Inorg. Chem. 2016, 55, 4545–4554. [Google Scholar] [CrossRef] [PubMed]
- Bolze, F.; Jenni, S.; Sour, A.; Heitz, V. Molecular photosensitisers for two-photon photodynamic therapy. Chem. Commun. 2017, 53, 12857–12877. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Zhang, L.-P.; Wu, F.; Zhao, Y. Photosensitizers for Two-Photon Excited Photodynamic Therapy. Adv. Funct. Mater. 2017, 27, 1704079. [Google Scholar] [CrossRef]
- Schmitt, J.; Heitz, V.; Sour, A.; Bolze, F.; Kessler, P.; Flamigni, L.; Ventura, B.; Bonnet, C.S.; Tóth, É. A Theranostic Agent Combining a Two-Photon-Absorbing Photosensitizer for Photodynamic Therapy and a Gadolinium(III) Complex for MRI Detection. Chem. Eur. J. 2016, 22, 2775–2786. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, J.; Jenni, S.; Sour, A.; Heitz, V.; Bolze, F.; Pallier, A.; Bonnet, C.S.; Tóth, É.; Ventura, B. A Porphyrin Dimer–GdDOTA Conjugate as a Theranostic Agent for One- and Two-Photon Photodynamic Therapy and MRI. Bioconj. Chem. 2018, 29, 3726–3738. [Google Scholar] [CrossRef] [PubMed]










© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jenni, S.; Sour, A. Molecular Theranostic Agents for Photodynamic Therapy (PDT) and Magnetic Resonance Imaging (MRI). Inorganics 2019, 7, 10. https://doi.org/10.3390/inorganics7010010
Jenni S, Sour A. Molecular Theranostic Agents for Photodynamic Therapy (PDT) and Magnetic Resonance Imaging (MRI). Inorganics. 2019; 7(1):10. https://doi.org/10.3390/inorganics7010010
Chicago/Turabian StyleJenni, Sébastien, and Angélique Sour. 2019. "Molecular Theranostic Agents for Photodynamic Therapy (PDT) and Magnetic Resonance Imaging (MRI)" Inorganics 7, no. 1: 10. https://doi.org/10.3390/inorganics7010010
APA StyleJenni, S., & Sour, A. (2019). Molecular Theranostic Agents for Photodynamic Therapy (PDT) and Magnetic Resonance Imaging (MRI). Inorganics, 7(1), 10. https://doi.org/10.3390/inorganics7010010