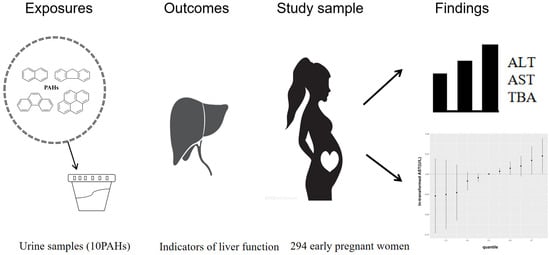
Single and Joint Associations of Polycyclic Aromatic Hydrocarbon Exposure with Liver Function during Early Pregnancy
Abstract
:1. Introduction
2. Methods and Materials
2.1. Study Population
2.2. Measurement of Urinary PAH Metabolite Concentrations
2.3. Assessment of Liver Function Markers
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics of the Pregnant Woman
3.2. Distributions of Urinary PAH Metabolites and Liver Function Indicators
3.3. Single Associations between Urinary PAH Metabolites and Liver Function Parameters
3.4. The Joint Association of PAH Metabolites on Liver Function Based on the BKMR Model
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Meah, V.L.; Cockcroft, J.R.; Backx, K.; Shave, R.; Stohr, E.J. Cardiac output and related haemodynamics during pregnancy: A series of meta-analyses. Heart 2016, 102, 518–526. [Google Scholar] [PubMed]
- Melchiorre, K.; Sharma, R.; Khalil, A.; Thilaganathan, B. Maternal Cardiovascular Function in Normal Pregnancy: Evidence of Maladaptation to Chronic Volume Overload. Hypertension 2016, 67, 754–762. [Google Scholar] [CrossRef] [PubMed]
- Bacq, Y.; Zarka, O.; Brechot, J.F.; Mariotte, N.; Vol, S.; Tichet, J.; Weill, J. Liver function tests in normal pregnancy: A prospective study of 103 pregnant women and 103 matched controls. Hepatology 1996, 23, 1030–1034. [Google Scholar] [CrossRef] [PubMed]
- Lao, T.T. Implications of abnormal liver function in pregnancy and non-alcoholic fatty liver disease. Best Pr. Res. Cl. Ob. 2020, 68, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Tran, T.T.; Ahn, J.; Reau, N.S. ACG Clinical Guideline: Liver Disease and Pregnancy. Am. J. Gastroenterol. 2016, 111, 196. [Google Scholar]
- Yarrington, C.D.; Cantonwine, D.E.; Seely, E.W.; McElrath, T.F.; Zera, C.A. The Association of Alanine Aminotransferase in Early Pregnancy with Gestational Diabetes. Metab. Syndr. Relat. Disord. 2016, 14, 254–258. [Google Scholar] [CrossRef]
- Mei-Dan, E.; Wiznitzer, A.; Sergienko, R.; Hallak, M.; Sheiner, E. Prediction of preeclampsia: Liver function tests during the first 20 gestational weeks. J. Matern. Fetal Neo. Med. 2013, 26, 250–253. [Google Scholar] [CrossRef]
- Faulkes, R.E.; Chauhan, A.; Knox, E.; Johnston, T.; Thompson, F.; Ferguson, J. Review article: Chronic liver disease and pregnancy. Aliment. Pharm. Ther. 2020, 52, 42042–42049. [Google Scholar] [CrossRef]
- Zhu, J.; Zhao, L.Y.; Wang, X.X.; Shi, Z.; Zhang, Y.; Wu, G.; Zhang, S.Y. Identification of hepatotoxicity and renal dysfunction of pyrene in adult male rats. Environ. Toxicol. 2018, 33, 1304–1311. [Google Scholar] [CrossRef]
- Yu, L.; Yang, M.; Cheng, M.; Fan, L.; Wang, X.; Xu, T.; Wang, B.; Chen, W. Associations between urinary phthalate metabolite concentrations and markers of liver injury in the US adult population. Environ. Int. 2021, 155, 106608. [Google Scholar] [CrossRef]
- Gao, P.; Da, S.E.; Hou, L.; Denslow, N.D.; Xiang, P.; Ma, L.Q. Human exposure to polycyclic aromatic hydrocarbons: Metabolomics perspective. Environ. Int. 2018, 119, 466–477. [Google Scholar] [CrossRef] [PubMed]
- Moorthy, B.; Chu, C.; Carlin, D.J. Polycyclic aromatic hydrocarbons: From metabolism to lung cancer. Toxicol. Sci. 2015, 145, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Cathey, A.L.; Watkins, D.J.; Rosario, Z.Y.; Velez, V.C.; Loch-Caruso, R.; Alshawabkeh, A.N.; Cordero, J.F.; Meeker, J.D. Polycyclic aromatic hydrocarbon exposure results in altered CRH, reproductive, and thyroid hormone concentrations during human pregnancy. Sci. Total Environ. 2020, 749, 141581. [Google Scholar] [CrossRef] [PubMed]
- Yang, P.; Gong, Y.J.; Cao, W.C.; Wang, R.X.; Wang, Y.X.; Liu, C.; Chen, Y.-J.; Huang, L.-L.; Ai, S.-H.; Lu, W.-Q.; et al. Prenatal urinary polycyclic aromatic hydrocarbon metabolites, global DNA methylation in cord blood, and birth outcomes: A cohort study in China. Environ. Pollut. 2018, 234, 396–405. [Google Scholar] [CrossRef]
- Hu, Z.; Li, Y.; Yang, Y.; Yu, W.; Xie, W.; Song, G.; Qian, Y.; Song, Z. Serum lipids mediate the relationship of multiple polyaromatic hydrocarbons on non-alcoholic fatty liver disease: A population-based study. Sci. Total Environ. 2021, 780, 146563. [Google Scholar] [CrossRef]
- Zheng, J.; Zheng, W.; Zhou, Y.; Jiang, S.; Spencer, P.; Ye, W.; Zheng, Y.; He, G.; Qu, W. Heavy Exposure of Waste Collectors to Polycyclic Aromatic Hydrocarbons in a Poor Rural Area of Middle China. Environ. Sci. Technol. 2018, 52, 8866–8875. [Google Scholar] [CrossRef]
- Xu, C.; Liu, Q.; Liang, J.; Weng, Z.; Xu, J.; Jiang, Z.; Gu, A. Urinary biomarkers of polycyclic aromatic hydrocarbons and their associations with liver function in adolescents. Environ. Pollut. 2021, 278, 116842. [Google Scholar] [CrossRef]
- Tian, Y.; Zhang, R.; Liu, X.; Liu, Y.; Xiong, S.; Wang, X.; Zhang, H.; Li, Q.; Liao, J.; Fang, D.; et al. Characteristics of exposure to 10 polycyclic aromatic hydrocarbon metabolites among pregnant women: Cohort of pregnant women in Zunyi, southwest China. Occup. Environ. Med. 2023, 80, 34–41. [Google Scholar] [CrossRef]
- Robles-Diaz, M.; Garcia-Cortes, M.; Medina-Caliz, I.; Gonzalez-Jimenez, A.; Gonzalez-Grande, R.; Navarro, J.M.; Castiella, A.; Zapata, E.M.; Romero-Gomez, M.; Blanco, S.; et al. The value of serum aspartate aminotransferase and gamma-glutamyl transpetidase as biomarkers in hepatotoxicity. Liver Int. 2015, 35, 2474–2482. [Google Scholar] [CrossRef]
- Wahlstrom, A.; Sayin, S.I.; Marschall, H.U.; Backhed, F. Intestinal Crosstalk between Bile Acids and Microbiota and Its Impact on Host Metabolism. Cell. Metab. 2016, 24, 41–50. [Google Scholar] [CrossRef]
- Zota, A.R.; Phillips, C.A.; Mitro, S.D. Recent Fast Food Consumption and Bisphenol A and Phthalates Exposures among the U.S. Population in NHANES, 2003–2010. Environ. Health Persp. 2016, 124, 1521–1528. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Xu, J.; Zhang, X.; Xu, S.; Liu, Q.; Weng, Z.; Gu, A. Serum nickel is associated with craniosynostosis risk: Evidence from humans and mice. Environ. Int. 2021, 146, 106289. [Google Scholar] [CrossRef]
- Andaluri, G.; Manickavachagam, M.; Suri, R. Plastic toys as a source of exposure to bisphenol-A and phthalates at childcare facilities. Environ. Monit. Assess. 2018, 190, 65. [Google Scholar] [CrossRef] [PubMed]
- Czaplicka, M. Sources and transformations of chlorophenols in the natural environment. Sci. Total Environ. 2004, 322, 21–39. [Google Scholar] [CrossRef] [PubMed]
- Wittassek, M.; Koch, H.M.; Angerer, J.; Bruning, T. Assessing exposure to phthalates—The human biomonitoring approach. Mol. Nutr. Food Res. 2011, 55, 7–31. [Google Scholar] [CrossRef]
- Bobb, J.F.; Valeri, L.; Claus, H.B.; Christiani, D.C.; Wright, R.O.; Mazumdar, M.; Godleski, J.J.; Coull, B.A. Bayesian kernel machine regression for estimating the health effects of multi-pollutant mixtures. Biostatistics 2015, 16, 493–508. [Google Scholar] [CrossRef]
- Coull, B.A.; Bobb, J.F.; Wellenius, G.A.; Kioumourtzoglou, M.A.; Mittleman, M.A.; Koutrakis, P.; Godleski, J.J. Part 1. Statistical Learning Methods for the Effects of Multiple Air Pollution Constituents. Res. Rep. Health Eff. Inst. 2015, 183, 5–50. [Google Scholar]
- Coker, E.; Chevrier, J.; Rauch, S.; Bradman, A.; Obida, M.; Crause, M.; Bornman, R.; Eskenazi, B. Corrigendum to “Association between prenatal exposure to multiple insecticides and child body weight and body composition in the VHEMBE South African birth cohort”. Environ. Int. 2018, 113, 122–132, Erratum in Environ. Int. 2020, 143, 106070. [Google Scholar] [CrossRef]
- Mikheev, M.I.; Lowry, L.K. WHO global project on biological monitoring of chemical exposure at the workplace. Int. Arch. Occ. Environ. Health 1996, 68, 387–388. [Google Scholar] [CrossRef]
- Newsome, P.N.; Cramb, R.; Davison, S.M.; Dillon, J.F.; Foulerton, M.; Godfrey, E.M.; Hall, R.; Harrower, U.; Hudson, M.; Langford, A.; et al. Guidelines on the management of abnormal liver blood tests. Gut 2018, 67, 6–19. [Google Scholar] [CrossRef]
- Gallo, V.; Leonardi, G.; Genser, B.; Lopez-Espinosa, M.J.; Frisbee, S.J.; Karlsson, L.; Ducatman, A.M.; Fletcher, T. Serum perfluorooctanoate (PFOA) and perfluorooctane sulfonate (PFOS) concentrations and liver function biomarkers in a population with elevated PFOA exposure. Environ. Health Persp. 2012, 120, 655–660. [Google Scholar] [CrossRef] [PubMed]
- Hassen, F.S.; Malik, T.; Dejenie, T.A. Evaluation of serum uric acid and liver function tests among pregnant women with and without preeclampsia at the University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia. PLoS ONE 2022, 17, e272165. [Google Scholar] [CrossRef] [PubMed]
- Min, Y.S.; Lim, H.S.; Kim, H. Biomarkers for polycyclic aromatic hydrocarbons and serum liver enzymes. Am. J. Ind. Med. 2015, 58, 764–772. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, T.; Ruhr, L.P.; Flory, W.; Giamalva, D.; Church, D.F.; Pryor, W.A. Toxicity of polycyclic aromatic hydrocarbons. I. Effect of phenanthrene, pyrene, and their ozonized products on blood chemistry in rats. Toxicol. Appl. Pharm. 1985, 79, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Sun, R.; Li, Y.; Chen, H.; Wu, L.; Shen, S.; Wei, Y.; Wang, N.; Zhang, Z.; Liu, Z.; et al. Changes in serum total bile acid concentrations are associated with the risk of developing adverse maternal and perinatal outcomes in pregnant Chinese women. Clin. Chim. Acta 2021, 520, 160–167. [Google Scholar] [CrossRef]
- Xu, Q.; Hu, L.; Chen, S.; Fu, X.; Gong, P.; Huang, Z.; Miao, W.; Jin, C.; Jin, Y. Parental exposure 3-methylcholanthrene disturbed the enterohepatic circulation in F1 generation of mice. Chemosphere 2022, 286, 131681. [Google Scholar] [CrossRef]
- Goedtke, L.; Sprenger, H.; Hofmann, U.; Schmidt, F.F.; Hammer, H.S.; Zanger, U.M.; Poetz, O.; Seidel, A.; Braeuning, A.; Hessel-Pras, S. Polycyclic Aromatic Hydrocarbons Activate the Aryl Hydrocarbon Receptor and the Constitutive Androstane Receptor to Regulate Xenobiotic Metabolism in Human Liver Cells. Int. J. Mol. Sci. 2020, 22, 372. [Google Scholar] [CrossRef]
- Tao, L.P.; Li, X.; Zhao, M.Z.; Shi, J.R.; Ji, S.Q.; Jiang, W.Y.; Liang, Q.-J.; Lei, Y.-H.; Zhou, Y.-Y.; Cheng, R.; et al. Chrysene, a four-ring polycyclic aromatic hydrocarbon, induces hepatotoxicity in mice by activation of the aryl hydrocarbon receptor (AhR). Chemosphere 2021, 276, 130108. [Google Scholar] [CrossRef]
- Malin, A.J.; Lesseur, C.; Busgang, S.A.; Curtin, P.; Wright, R.O.; Sanders, A.P. Fluoride exposure and kidney and liver function among adolescents in the United States: NHANES, 2013–2016. Environ. Int. 2019, 132, 105012. [Google Scholar] [CrossRef]
- Cichoz-Lach, H.; Michalak, A. Oxidative stress as a crucial factor in liver diseases. World J. Gastroenterol. 2014, 20, 8082–8091. [Google Scholar] [CrossRef]
- Perez-Umphrey, A.A.; Bergeon, B.C.; Stouffer, P.C.; Woltmann, S.; Taylor, S.S. Polycyclic aromatic hydrocarbon exposure in seaside sparrows (Ammodramus maritimus) following the 2010 Deepwater Horizon oil spill. Sci. Total Environ. 2018, 630, 1086–1094. [Google Scholar] [CrossRef]
- Yazdani, M. Comparative toxicity of selected PAHs in rainbow trout hepatocytes: Genotoxicity, oxidative stress, and cytotoxicity. Drug Chem. Toxicol. 2020, 43, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.J.; Kim, S.; Choi, S.; Lee, I.; Moon, M.K.; Choi, K.; Park, Y.J.; Cho, Y.H.; Kwon, Y.M.; Yoo, J.; et al. Association of exposure to polycyclic aromatic hydrocarbons and heavy metals with thyroid hormones in general adult population and potential mechanisms. Sci. Total Environ. 2021, 762, 144227. [Google Scholar] [CrossRef] [PubMed]
- Luo, C.; Deng, J.; Chen, L.; Wang, Q.; Xu, Y.; Lyu, P.; Zhou, L.; Shi, Y.; Mao, W.; Yang, X.; et al. Phthalate acid esters and polycyclic aromatic hydrocarbons concentrations with their determining factors among Chinese pregnant women: A focus on dietary patterns. Sci. Total Environ. 2022, 852, 158344. [Google Scholar] [CrossRef] [PubMed]
- Yi, W.; Cheng, J.; Song, J.; Pan, R.; Liang, Y.; Sun, X.; Li, Y.; Wu, Y.; Yan, S.; Jin, X.; et al. Associations of polycyclic aromatic hydrocarbons, water-soluble ions and metals in PM (2.5) with liver function: Evidence from schizophrenia cohort. Sci. Total Environ. 2023, 868, 161624. [Google Scholar] [CrossRef] [PubMed]



| Characteristics | Mean (SD) or n (%) |
|---|---|
| Age (years) | 26.36 ± 4.78 |
| Pre-pregnancy BMI | 22.50 ± 4.85 |
| Parity | |
| 0 | 100 (34) |
| ≥1 | 194 (66) |
| Education | |
| Less than high school | 171 (58.2) |
| High school and above | 123 (41.8) |
| Household income (RMB yuan/year) | |
| <100,000 | 35 (11.9) |
| 100,000–150,000 | 196 (66.7) |
| ≥150,000 | 38 (12.8) |
| Unknown | 25 (8.4) |
| Passive smoking | |
| Yes | 284 (96.9) |
| No | 10 (3.4) |
| Physical activity | |
| Never | 122 (41.5) |
| 1–2 times/week | 39 (13.3) |
| ≥3 times/week | 133 (45.2) |
| Ethnicity | |
| The Han nationality | 293 (99.7) |
| Other | 1 (0.3) |
| Gestational hypertension disorder | |
| Yes | 1 (0.3) |
| No | 293 (99.7) |
| Gestational diabetes mellitus | |
| Yes | 0 (0) |
| No | 294 (100) |
| Analyte (µg/g) | Percent Detection | Medians, 25th and 75th Percentile |
|---|---|---|
| 1-OH-PHE | 83.33% | 0.09 (0.02, 0.26) |
| 2-OH-PHE | 76.53% | 0.09 (0.01, 0.55) |
| 3-OH-PHE | 92.52% | 0.28 (0.09, 0.73) |
| 4-OH-PHE | 63.27% | 0.03 (0.01, 0.07) |
| 9-OH-PHE | 85.37% | 0.02 (0.01, 0.05) |
| 1-OH-NAP | 64.97% | 0.57 (<LOD, 2.05) |
| 2-OH-NAP | 79.59% | 0.98 (0.05, 4.49) |
| 2-OH-FLU | 99.32% | 0.55 (0.25, 0.98) |
| 9-OH-FLU | 88.78% | 0.37 (0.15, 0.80) |
| 1-OH-PYR | 71.77% | 0.01 (<LOD, 0.07) |
| Liver function parameters (U/L) | ||
| ALT | - | 12.00 (9.00, 18.75) |
| AST | - | 18.00 (15.50, 21.25) |
| ALP | - | 59.50 (47.00, 76.00) |
| TBA | - | 2.00 (1.30, 3.30) |
| AST/ALT | - | 1.42 (1.05, 1.75) |
| Analyte (µg/g) | ALT | AST | ||
|---|---|---|---|---|
| %Δ (95% CI) | p-Value | %Δ (95% CI) | p-Value | |
| 1-OHPHE | 0.70 (−3.15, 4.71) | 0.728 | 0.60(−1.29, 2.63) | 0.530 |
| 2-OHPHE | 3.36 (0.40, 6.40) | 0.026 | 2.22 (0.80, 3.67) | 0.003 |
| 3-OHPHE | 0.90 (−2.86, 4.92) | 0.633 | 0.70 (−1.19, 2.74) | 0.456 |
| 4-OHPHE | 3.67 (−1.98, 9.64) | 0.201 | 2.43 (−0.40, 5.23) | 0.097 |
| 9-OHPHE | 1.82 (−2.86, 6.72) | 0.446 | 1.82 (−0.50, 4.19) | 0.131 |
| 2-OHFLU | 0.20 (−5.26, 5.97) | 0.948 | 0.50 (−2.27, 3.36) | 0.711 |
| 9-OHFLU | 1.41 (−1.88, 4.81) | 0.410 | 1.21 (−0.40, 2.94) | 0.153 |
| 1-OHNAP | 0.50 (−1.69, 2.74) | 0.654 | 0.70 (−0.50, 1.82) | 0.244 |
| 2-OHNAP | −0.20 (−2.37, 2.12) | 0.880 | 0.40 (−0.80, 1.51) | 0.530 |
| 1-OHPYR | −0.80 (−3.05, 1.51) | 0.492 | −0.50 (−1.69, 0.60) | 0.356 |
| ALP | TBA | |||
| %Δ (95% CI) | p-value | %Δ (95% CI) | p-value | |
| 1-OHPHE | 0.10 (−2.76, 3.15) | 0.931 | 7.04 (1.61, 12.75) | 0.011 |
| 2-OHPHE | −1.49 (−3.63, 0.60) | 0.167 | 0.30 (−3.63, 4.29) | 0.900 |
| 3-OHPHE | 0.70 (−2.18, 3.67) | 0.648 | −1.98 (−7.04, 3.25) | 0.442 |
| 4-OHPHE | 0.50 (−3.63, 4.81) | 0.818 | 6.08 (−1.69, 14.34) | 0.127 |
| 9-OHPHE | −1.39 (−4.78, 2.12) | 0.441 | −1.49 (−7.50, 5.02) | 0.650 |
| 2-OHFLU | −0.40 (−4.50, 3.87) | 0.839 | −1.78 (−8.88, 5.87) | 0.639 |
| 9-OHFLU | −0.70 (−3.15, 1.82) | 0.561 | 2.43 (−2.08, 7.14) | 0.287 |
| 1-OHNAP | −0.50 (−2.18, 1.11) | 0.527 | 1.21 (−1.78, 4.29) | 0.431 |
| 2-OHNAP | −1.39 (−3.05, 0.30) | 0.114 | −1.59 (−4.50, 1.51) | 0.314 |
| 1-OHPYR | −0.50 (−2.18, 1.21) | 0.590 | −0.20 (−3.25, 2.94) | 0.913 |
| AST/ALT | ||||
| %Δ (95% CI) | p-value | |||
| 1-OHPHE | −0.10 (−2.76, 2.74) | 0.970 | ||
| 2-OHPHE | −1.09 (−3.05, 0.9) | 0.283 | ||
| 3-OHPHE | −0.20 (−2.86, 2.53) | 0.865 | ||
| 4-OHPHE | −1.39 (−5.16, 2.63) | 0.495 | ||
| 9-OHPHE | −0.20 (−3.44, 3.15) | 0.906 | ||
| 2-OHFLU | 0.30 (3.67, 4.29) | 0.866 | ||
| 9-OHFLU | −0.20 (−2.47, 2.12) | 0.885 | ||
| 1-OHNAP | 0.10 (−1.49, 1.61) | 0.921 | ||
| 2-OHNAP | 0.60 (−1.00, 2.12) | 0.491 | ||
| 1-OHPYR | 0.30 (−1.29, 1.92) | 0.730 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dai, M.; Luo, L.; Xie, C.; Chen, Z.; Zhang, M.; Xie, Y.; Shang, X.; Shen, X.; Tian, K.; Zhou, Y. Single and Joint Associations of Polycyclic Aromatic Hydrocarbon Exposure with Liver Function during Early Pregnancy. Toxics 2023, 11, 863. https://doi.org/10.3390/toxics11100863
Dai M, Luo L, Xie C, Chen Z, Zhang M, Xie Y, Shang X, Shen X, Tian K, Zhou Y. Single and Joint Associations of Polycyclic Aromatic Hydrocarbon Exposure with Liver Function during Early Pregnancy. Toxics. 2023; 11(10):863. https://doi.org/10.3390/toxics11100863
Chicago/Turabian StyleDai, Mi, Lei Luo, Caiyan Xie, Zhongbao Chen, Mingzhe Zhang, Yan Xie, Xuejun Shang, Xubo Shen, Kunming Tian, and Yuanzhong Zhou. 2023. "Single and Joint Associations of Polycyclic Aromatic Hydrocarbon Exposure with Liver Function during Early Pregnancy" Toxics 11, no. 10: 863. https://doi.org/10.3390/toxics11100863
APA StyleDai, M., Luo, L., Xie, C., Chen, Z., Zhang, M., Xie, Y., Shang, X., Shen, X., Tian, K., & Zhou, Y. (2023). Single and Joint Associations of Polycyclic Aromatic Hydrocarbon Exposure with Liver Function during Early Pregnancy. Toxics, 11(10), 863. https://doi.org/10.3390/toxics11100863