Emerging Trends in the Application of Green Synthesized Biocompatible ZnO Nanoparticles for Translational Paradigm in Cancer Therapy
Abstract
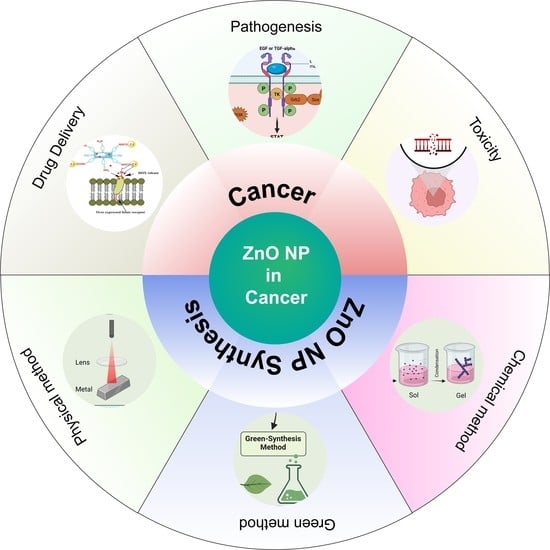
:1. Introduction
2. Zinc Oxide Nanoparticles and Their Physiochemical Properties
2.1. Size and Shape
2.1.1. One-Dimensional (1D)
2.1.2. Two-Dimensional (2D)
2.1.3. Three-Dimensional (3D)
2.2. Surface Area
2.3. Electrical and Optical Properties
2.4. Thermal Stability
2.5. Magnetic Properties
2.6. ROS Inducing Property
3. Synthesis of Zinc Oxide Nanoparticles
3.1. Physical Methods
3.2. Chemical Methods
3.3. Bio-Synthesis
3.3.1. Plant-Mediated Synthesis
| Plants Used for Green Synthesis | Plant Part Used for Synthesis | Morphology of ZnO Nanoparticles | Size Range (nm) | References |
|---|---|---|---|---|
| Myristica fragrans | Fruit Extracts | Spherical- to hexagonal-shaped particles | 43.3 to 83.1 nm (SEM) | [78] |
| Cassia fistula | Leaf extracts | Spherical/agglomerated | 0.1 nm to 10,000 nm (SEM) | [79] |
| Melia azadarach | Leaf extracts | Spherical/agglomerated | 0.1 nm to 10,000 nm (SEM) | [79] |
| Elaeagnus angustifolia | Leaf extracts | Spherical/agglomerated | ~26 nm (TEM) | [80] |
| Geranium wallichianum | Leaf Extracts | Hexagonal | ~18 nm (TEM) | [81] |
| Euphorbia heterophylla (L.) | Leaf Extracts | Hexagonal | ~40 nm (SEM) | [82] |
| Moringa oleifera | Gum | Agglomerated | ~60 nm (SEM) | [83] |
| Azadirachta indica | Leaf Extracts | Hexagonal | 10–30 nm (TEM) | [84] |
| Azadirachta indica | Leaf Extracts | Spherical | 18 nm (XRD) | [85] |
| Agathosma betulina | Leaf Extracts | Quasi-spherical agglomerates | 15.8 nm (TEM), 12–26 nm (HRTEM) | [86] |
| Rosa canina | Fruit extract | Spherical | <50 nm (SEM) | [87] |
| Cocus nucifera | Coconut water | Spherical and predominantly hexagonal without any agglomeration | 20–80 nm (TEM), 21.2 nm (XRD) | [87] |
| Vitex negundo | Flowers | Hexagonal | 38.17 nm (XRD) | [88] |
| Vitex negundo | Leaf Extracts | Spherical | 75–80 nm (SEM & EDX), 38.17nm (XRD) | [88] |
| Solanum nigrum | Leaf extract | Wurtzite hexagonal, quasi-spherical | 20–30 nm (XRD and FE-SEM), 29.79 nm (TEM) | [89] |
| Gossypium | Cellulosic fiber | Wurtzite, spherical, nano rod | 13 nm (XRD) | [89] |
| Pongamia pinnata | Fresh leaves | Spherical, hexagonal, nano rod | 26 nm (XRD), Agglomeration of 100 nm (DLS, SEM, TEM) | [88] |
| Plectranthus amboinicus | Leaf extract | Rod shape nanoparticle with agglomerates | 50–180 nm (SEM) | [90] |
| Phyllanthus niruri | Leaf Extracts | Hexagonal wurtzite, quasi-spherical | 25.61 nm (FE-SEM & XRD) | [91] |
| Nephelium lappaceum L. | Fruit peels | Needle-shaped forming agglomerate | 50.95 nm (XRD) | [92] |
| Anisochilus carnosus | Leaf extract | Hexagonal wurtzite, quasi-spherical | 20–40 nm (FE-SEM), 30–40 nm (TEM) | [93] |
| Trifolium pratense | Flower Extract | Spherical | 60–70 nm (XRD) | [94] |
| Aloe vera | Freeze-dried leaf peel | Spherical, hexagonal | 25–65 nm (SEM & TEM) | [95] |
3.3.2. Microbial-Mediated Synthesis
4. Toxicology Concerns of ZnO Nanoparticles
4.1. Pulmonary Toxicity
4.2. Genotoxicity
4.3. Neurotoxicity
4.4. Reproductive Toxicity

5. Pathogenesis of Cancer
6. Drug Delivery
7. Future Perspective
8. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Gomez, G.G.; Wykosky, J.; Zanca, C.; Furnari, F.B.; Cavenee, W.K. Therapeutic resistance in cancer: microRNA regulation of EGFR signaling networks. Cancer Biol. Med. 2013, 10, 192–205. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Z.; Li, M.; Dey, R.; Chen, Y. Nanomaterials for cancer therapy: Current progress and perspectives. J. Hematol. Oncol. 2021, 14, 85. [Google Scholar] [CrossRef] [PubMed]
- Mishra, Y.K.; Adelung, R. ZnO tetrapod materials for functional applications. Mater. Today 2018, 21, 631–651. [Google Scholar] [CrossRef]
- Bisht, G.; Rayamajhi, S. ZnO Nanoparticles: A Promising Anticancer Agent. Nanobiomedicine 2016, 3, 9. [Google Scholar] [CrossRef]
- Lu, X.; Zhu, T.; Chen, C.; Liu, Y. Right or Left: The Role of Nanoparticles in Pulmonary Diseases. Int. J. Mol. Sci. 2014, 15, 17577–17600. [Google Scholar] [CrossRef] [Green Version]
- Jiang, J.; Pi, J.; Cai, J. The Advancing of Zinc Oxide Nanoparticles for Biomedical Applications. Bioinorg. Chem. Appl. 2018, 2018, 1062562. [Google Scholar] [CrossRef]
- Choi, S.J.; Choy, J.H. Biokinetics of zinc oxide nanoparticles: Toxicokinetics, biological fates, and protein interaction. Int. J. Nanomed. 2014, 9, 261–269. [Google Scholar] [CrossRef] [Green Version]
- Anjum, S.; Hashim, M.; Malik, S.A.; Khan, M.; Lorenzo, J.M.; Abbasi, B.H.; Hano, C. Recent Advances in Zinc Oxide Nanoparticles (ZnO NPs) for Cancer Diagnosis, Target Drug Delivery, and Treatment. Cancers 2021, 13, 4570. [Google Scholar] [CrossRef]
- Hahm, J. Fundamental Properties of One-Dimensional Zinc Oxide Nanomaterials and Implementations in Various Detection Modes of Enhanced Biosensing. Annu. Rev. Phys. Chem. 2016, 67, 691–717. [Google Scholar] [CrossRef] [Green Version]
- Shah, A.; Aftab, S.; Nisar, J.; Ashiq, M.N.; Iftikhar, F.J. Nanocarriers for targeted drug delivery. J. Drug Deliv. Sci. Technol. 2021, 62, 102426. [Google Scholar] [CrossRef]
- Zhou, G.; Latchoumanin, O.; Hebbard, L.; Duan, W.; Liddle, C.; George, J.; Qiao, L. Aptamers as targeting ligands and therapeutic molecules for overcoming drug resistance in cancers. Adv. Drug Deliv. Rev. 2018, 134, 107–121. [Google Scholar] [CrossRef] [PubMed]
- Fraceto, L.F.; Campos, E.V.R.; Habtemariam, S.; del Rodriguez-Torres, M.P.; Patra, J.K.; Grillo, R.; Acosta-Torres, L.S.; Sharma, S.; Shin, H.-S.; Diaz-Torres, L.A.; et al. Nano based drug delivery systems: Recent developments and future prospects. J. Nanobiotechnol. 2018, 16, 71. [Google Scholar]
- Makkar, H.; Verma, S.K.; Panda, P.K.; Pramanik, N.; Jha, E.; Suar, M. Molecular insight to size and dose-dependent cellular toxicity exhibited by a green synthesized bioceramic nanohybrid with macrophages for dental applications. Toxicol. Res. 2018, 7, 959–969. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, Y.; Li, Y.; Xu, Q.; Liu, Z. Mesoporous silica nanoparticles for stimuli-responsive controlled drug delivery: Advances, challenges, and outlook. Int. J. Nanomed. 2016, 12, 87–110. [Google Scholar] [CrossRef] [Green Version]
- Fernandes, N.B.; Nayak, Y.; Garg, S.; Nayak, U.Y. Multifunctional engineered mesoporous silica/inorganic material hybrid nanoparticles: Theranostic perspectives. Coord. Chem. Rev. 2023, 478. [Google Scholar] [CrossRef]
- Xie, J.; Li, H.; Zhang, T.; Song, B.; Wang, X.; Gu, Z. Recent Advances in ZnO Nanomaterial-Mediated Biological Applications and Action Mechanisms. Nanomaterials 2023, 13, 1500. [Google Scholar] [CrossRef]
- Hou, C.-C.; Zhu, J.-Q. Nanoparticles and female reproductive system: How do nanoparticles affect oogenesis and embryonic development. Oncotarget 2017, 8, 109799–109817. [Google Scholar] [CrossRef] [Green Version]
- Raj, V.J.; Ghosh, R.; Girigoswami, A.; Girigoswami, K. Application of zinc oxide nanoflowers in environmental and biomedical science. BBA Adv. 2022, 2, 100051. [Google Scholar] [CrossRef]
- Mohd Yusof, H.; Mohamad, R.; Zaidan, U.H.; Abdul Rahman, N.A. Microbial synthesis of zinc oxide nanoparticles and their potential application as an antimicrobial agent and a feed supplement in animal industry: A review. J. Anim. Sci. Biotechnol. 2019, 10, 57. [Google Scholar] [CrossRef] [Green Version]
- Kumari, P.; Misra, K.P.; Chattopadhyay, S.; Samanta, S. A brief review on transition metal ion doped ZnO nanoparticles and its optoelectronic applications. Mater. Today Proc. 2021, 43, 3297–3302. [Google Scholar] [CrossRef]
- Li, Y.; Yang, X.-Y.; Feng, Y.; Yuan, Z.-Y.; Su, B.-L. One-Dimensional Metal Oxide Nanotubes, Nanowires, Nanoribbons, and Nanorods: Synthesis, Characterizations, Properties and Applications. Crit. Rev. Solid State Mater. Sci. 2012, 37, 606512. [Google Scholar] [CrossRef]
- Mourdikoudis, S.; Pallares, R.M.; Thanh, N.T.K. Characterization techniques for nanoparticles: Comparison and complementarity upon studying nanoparticle properties. Nanoscale 2018, 10, 12871–12934. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarkar, S.; Sarkar, R. Synthesis, characterization and tribological study of zinc oxide nanoparticles. Mater. Today Proc. 2021, 44, 3606–3612. [Google Scholar] [CrossRef]
- Moumen, A.; Kaur, N.; Poli, N.; Zappa, D.; Comini, E. One dimensional ZnO nanostructures: Growth and chemical sensing performances. Nanomaterials 2020, 10, 1940. [Google Scholar] [CrossRef]
- Jin, S.E.; Jin, H.E. Synthesis, characterization, and three-dimensional structure generation of zinc oxide-based nanomedicine for biomedical applications. Pharmaceutics 2019, 11, 575. [Google Scholar] [CrossRef] [Green Version]
- Mehrvarz, A.; Khalil-Allafi, J.; Khosrowshahi, A.K. Biocompatibility and antibacterial behavior of electrochemically deposited Hydroxyapatite/ZnO porous nanocomposite on NiTi biomedical alloy. Ceram. Int. 2022, 48, 16326–16336. [Google Scholar] [CrossRef]
- Kumar, S.; Shukla, M.K.; Sharma, A.K.; Jayaprakash, G.K.; Tonk, R.K.; Chellappan, D.K.; Singh, S.K.; Dua, K.; Ahmed, F.; Bhattacharyya, S.; et al. Metal-based nanomaterials and nanocomposites as promising frontier in cancer chemotherapy. MedComm 2023, 4. [Google Scholar] [CrossRef]
- Bashir, S.; Awan, M.S.; Farrukh, M.A.; Naidu, R.; Khan, S.A.; Rafique, N.; Ali, S.; Hayat, I.; Hussain, I.; Khan, M.Z. In-vivo (Albino Mice) and in-vitro Assimilation and Toxicity of Zinc Oxide Nanoparticles in Food Materials. Int. J. Nanomed. 2022, 17, 4073–4085. [Google Scholar] [CrossRef]
- Sullivan, I.; Zoellner, B.; Maggard, P.A. Copper(I)-Based p-Type Oxides for Photoelectrochemical and Photovoltaic Solar Energy Conversion. Chem. Mater. 2016, 28, 5999–6016. [Google Scholar] [CrossRef]
- Solati, E.; Dejam, L.; Dorranian, D. Effect of laser pulse energy and wavelength on the structure, morphology and optical properties of ZnO nanoparticles. Opt. Laser Technol. 2014, 58, 26–32. [Google Scholar] [CrossRef]
- Yoshikawa, A.; Matsunami, H.; Nanishi, Y. Development and Applications of Wide Bandgap Semiconductors. In Wide Bandgap Semiconductors; Springer: Berlin/Heidelberg, Germany, 2007; pp. 1–24. [Google Scholar]
- Sharma, D.K.; Shukla, S.; Sharma, K.K.; Kumar, V. A review on ZnO: Fundamental properties and applications. Mater. Today Proc. 2022, 49, 3028–3035. [Google Scholar] [CrossRef]
- Das, B.K.; Verma, S.K.; Das, T.; Panda, P.K.; Parashar, K.; Suar, M.; Parashar, S.K.S. Altered electrical properties with controlled copper doping in ZnO nanoparticles infers their cytotoxicity in macrophages by ROS induction and apoptosis. Chem. Biol. Interact. 2019, 297, 141–154. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.K.; Panda, P.K.; Jha, E.; Suar, M.; Parashar, S.K.S. Altered physiochemical properties in industrially synthesized ZnO nanoparticles regulate oxidative stress; Induce in vivo cytotoxicity in embryonic zebrafish by apoptosis. Sci. Rep. 2017, 7, 13909. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verma, S.K.; Suar, M.; Mishra, Y.K. Editorial: Green Perspective of Nano-Biotechnology: Nanotoxicity Horizon to Biomedical Applications. Front. Bioeng. Biotechnol. 2022, 10, 919226. [Google Scholar] [CrossRef]
- Verma, S.K.; Jha, E.; Kiran, K.J.; Bhat, S.; Suar, M.; Mohanty, P.S. Synthesis and characterization of novel polymer-hybrid silver nanoparticles and its biomedical study. Mater. Today Proc. 2016, 3, 1949–1957. [Google Scholar] [CrossRef]
- Krishnia, L.; Thakur, P.; Thakur, A. Synthesis of Nanoparticles by Physical Route. Synth. Appl. Nanopart. 2022, 45–59. [Google Scholar] [CrossRef]
- Paul, P.; Pattnaik, Y.; Panda, P.K.; Jha, E.; Verma, S.K.; Suar, M. Green Synthesized Metal Oxide Nanomaterials Photocatalysis in Combating Bacterial Infection. In Green Methods for Wastewater Treatment; Springer: Berlin/Heidelberg, Germany, 2020; pp. 73–86. [Google Scholar]
- Gudkov, S.V.; Burmistrov, D.E.; Serov, D.A.; Rebezov, M.B.; Semenova, A.A.; Lisitsyn, A.B. A Mini Review of Antibacterial Properties of ZnO Nanoparticles. Front. Phys. 2021, 9, 641481. [Google Scholar] [CrossRef]
- Abebe, B.; Zereffa, E.A.; Tadesse, A.; Murthy, H.C.A. A Review on Enhancing the Antibacterial Activity of ZnO: Mechanisms and Microscopic Investigation. Nanoscale Res. Lett. 2020, 15, 190. [Google Scholar] [CrossRef]
- Webster, T.J.; Seil, I. Antimicrobial applications of nanotechnology: Methods and literature. Int. J. Nanomed. 2012, 7, 2767–2781. [Google Scholar] [CrossRef] [Green Version]
- Verma, S.K.; Jha, E.; Panda, P.K.; Das, J.K.; Thirumurugan, A.; Suar, M.; Parashar, S.K.S. Molecular aspects of core-shell intrinsic defect induced enhanced antibacterial activity of ZnO nanocrystals. Nanomedicine 2018, 13, 43–68. [Google Scholar] [CrossRef]
- Gurunathan, S.; Kang, M.H.; Kim, J.H. Combination effect of silver nanoparticles and histone deacetylases inhibitor in human alveolar basal epithelial cells. Molecules 2018, 23, 2046. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mintcheva, N.; Aljulaih, A.A.; Wunderlich, W.; Kulinich, S.A.; Iwamori, S. Laser-Ablated ZnO nanoparticles and their photocatalytic activity toward organic pollutants. Materials 2018, 11, 1127. [Google Scholar] [CrossRef] [Green Version]
- Kim, M.; Osone, S.; Kim, T.; Higashi, H.; Seto, T. Synthesis of nanoparticles by laser ablation: A review. KONA Powder Part. J. 2017, 2017, 80–90. [Google Scholar] [CrossRef] [Green Version]
- Lv, H.; Sang, D.D.; Li, H.D.; Du, X.B.; Li, D.M.; Zou, G.T. Thermal Evaporation Synthesis and Properties of ZnO Nano/Microstructures Using Carbon Group Elements as the Reducing Agents. Nanoscale Res. Lett. 2010, 5, 620–624. [Google Scholar] [CrossRef] [Green Version]
- Sergievskaya, A.; Chauvin, A.; Konstantinidis, S. Sputtering onto liquids: A critical review. Beilstein J. Nanotechnol. 2022, 13, 10–53. [Google Scholar] [CrossRef] [PubMed]
- Wojnarowicz, J.; Chudoba, T.; Lojkowski, W. A Review of Microwave Synthesis of Zinc Oxide Nanomaterials: Reactants, Process Parameters and Morphologies. Nanomaterials 2020, 10, 1086. [Google Scholar] [CrossRef] [PubMed]
- Ba-Abbad, M.M.; Takriff, M.S.; Benamor, A.; Nasser, M.S.; Mahmoudi, E.; Mohammad, A.W. Synthesis and characterization of Sm3+-doped ZnO nanoparticles via a sol–gel method and their photocatalytic application. J. Sol-Gel Sci. Technol. 2018, 85, 178–190. [Google Scholar] [CrossRef]
- Marciello, M.; Luengo, Y.; Morales, M.P. Iron Oxide Nanoparticles for Cancer Diagnosis and Therapy. In Nanoarchitectonics for Smart Delivery and Drug Targeting; Elsevier: Amsterdam, The Netherlands, 2016; pp. 667–694. [Google Scholar]
- Baruah, S.; Dutta, J. Hydrothermal growth of ZnO nanostructures. Sci. Technol. Adv. Mater. 2009, 10, 013001. [Google Scholar] [CrossRef]
- Lee, K.-Y.; Pham, X.-H.; Rho, W.-Y.; Chang, H.; Lee, S.H.; Kim, J.; Hahm, E.; Lee, J.H.; Lee, Y.-S.; Jun, B.-H. Introduction of Nanobiotechnology. In Advances in Experimental Medicine and Biology; Springer: Berlin/Heidelberg, Germany, 2021; pp. 1–22. [Google Scholar]
- Bahrulolum, H.; Nooraei, S.; Javanshir, N.; Tarrahimofrad, H.; Mirbagheri, V.S.; Easton, A.J.; Ahmadian, G. Green synthesis of metal nanoparticles using microorganisms and their application in the agrifood sector. J. Nanobiotechnol. 2021, 19, 86. [Google Scholar] [CrossRef]
- Kuppusamy, P.; Yusoff, M.M.; Maniam, G.P.; Govindan, N. Biosynthesis of metallic nanoparticles using plant derivatives and their new avenues in pharmacological applications—An updated report. Saudi Pharm. J. 2016, 24, 473–484. [Google Scholar] [CrossRef]
- Sharma, D.; Kanchi, S.; Bisetty, K. Biogenic synthesis of nanoparticles: A review. Arab. J. Chem. 2019, 12, 3576–3600. [Google Scholar] [CrossRef] [Green Version]
- Singh, A.K. A review on plant extract-based route for synthesis of cobalt nanoparticles: Photocatalytic, electrochemical sensing and antibacterial applications. Curr. Res. Green Sustain. Chem. 2022, 5, 100270. [Google Scholar] [CrossRef]
- Antropova, I.G.; Revina, A.A.; Oo, P.M.; Kurakina, E.S.; Butorova, I.A.; Magomedbekov, E.P. Synthesis of Silver Nanoparticles Using Reactive Water-Ethanol Extracts from Murraya paniculata. ACS Omega 2021, 6, 8313–8321. [Google Scholar] [CrossRef]
- Kumari, P.; Panda, P.K.; Jha, E.; Kumari, K.; Nisha, K.; Mallick, M.A.; Verma, S.K. Mechanistic insight to ROS and Apoptosis regulated cytotoxicity inferred by Green synthesized CuO nanoparticles from Calotropis gigantea to Embryonic Zebrafish. Sci. Rep. 2017, 7, 16284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agarwal, H.; Venkat Kumar, S.; Rajeshkumar, S. A review on green synthesis of zinc oxide nanoparticles—An eco-friendly approach. Resour. Technol. 2017, 3, 406–413. [Google Scholar] [CrossRef]
- Verma, S.K.; Panda, P.K.; Kumari, P.; Patel, P.; Arunima, A.; Jha, E.; Husain, S.; Prakash, R.; Hergenröder, R.; Mishra, Y.K.; et al. Determining factors for the nano-biocompatibility of cobalt oxide nanoparticles: Proximal discrepancy in intrinsic atomic interactions at differential vicinage. Green Chem. 2021, 23, 3439–3458. [Google Scholar] [CrossRef]
- Gasmi, A.; Mujawdiya, P.K.; Noor, S.; Lysiuk, R.; Darmohray, R.; Piscopo, S.; Lenchyk, L.; Antonyak, H.; Dehtiarova, K.; Shanaida, M.; et al. Polyphenols in Metabolic Diseases. Molecules 2022, 27, 6280. [Google Scholar] [CrossRef]
- Kumari, K.; Nandi, A.; Sinha, A.; Panda, P.K.; Ghosh, A.; Gouda, S.K.; Suar, M.; Verma, S.K.; Raina, V. Biosurfactant-functionalized Silver nanoparticles infer intrinsic proximal interaction via Lysine and glutamic acid for reduced in vivo molecular biotoxicity with embryonic zebrafish through oxidative stress and apoptosis. J. Environ. Chem. Eng. 2023, 11, 110147. [Google Scholar] [CrossRef]
- Panda, P.K.; Kumari, P.; Patel, P.; Samal, S.K.; Mishra, S.; Tambuwala, M.M.; Dutt, A.; Hilscherová, K.; Mishra, Y.K.; Varma, R.S.; et al. Molecular nanoinformatics approach assessing the biocompatibility of biogenic silver nanoparticles with channelized intrinsic steatosis and apoptosis. Green Chem. 2022, 24, 1190–1210. [Google Scholar] [CrossRef]
- El Shafey, A.M. Green synthesis of metal and metal oxide nanoparticles from plant leaf extracts and their applications: A review. Green Process. Synth. 2020, 9, 304–339. [Google Scholar] [CrossRef]
- Akhtar, N.; Haq, I.U.; Mirza, B. Phytochemical analysis and comprehensive evaluation of antimicrobial and antioxidant properties of 61 medicinal plant species. Arab. J. Chem. 2018, 11, 1223–1235. [Google Scholar] [CrossRef] [Green Version]
- Sinha, A.; Simnani, F.Z.; Singh, D.; Nandi, A.; Choudhury, A.; Patel, P.; Jha, E.; Chouhan, R.S.; Kaushik, N.K.; Mishra, Y.K.; et al. The translational paradigm of nanobiomaterials: Biological chemistry to modern applications. Mater. Today Bio 2022, 17, 100463. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.K.; Jha, E.; Panda, P.K.; Thirumurugan, A.; Suar, M. Biological Effects of Green-Synthesized Metal Nanoparticles: A Mechanistic View of Antibacterial Activity and Cytotoxicity. In Advanced Nanostructured Materials for Environmental Remediation. Environmental Chemistry for a Sustainable World; Springer: Berlin/Heidelberg, Germany, 2019; pp. 145–171. [Google Scholar] [CrossRef]
- Priya; Naveen; Kaur, K.; Sidhu, A.K. Green Synthesis: An Eco-friendly Route for the Synthesis of Iron Oxide Nanoparticles. Front. Nanotechnol. 2021, 3, 655062. [Google Scholar] [CrossRef]
- Nava, O.J.; Soto-Robles, C.A.; Gómez-Gutiérrez, C.M.; Vilchis-Nestor, A.R.; Castro-Beltrán, A.; Olivas, A.; Luque, P.A. Fruit peel extract mediated green synthesis of zinc oxide nanoparticles. J. Mol. Struct. 2017, 1147, 1–6. [Google Scholar] [CrossRef]
- Matinise, N.; Fuku, X.G.; Kaviyarasu, K.; Mayedwa, N.; Maaza, M. ZnO nanoparticles via Moringa oleifera green synthesis: Physical properties & mechanism of formation. Appl. Surf. Sci. 2017, 406, 339–347. [Google Scholar] [CrossRef]
- Rajendran, N.K.; George, B.P.; Houreld, N.N.; Abrahamse, H. Synthesis of zinc oxide nanoparticles using rubus fairholmianus root extract and their activity against pathogenic bacteria. Molecules 2021, 26, 3029. [Google Scholar] [CrossRef]
- Singh, A.K.; Pal, P.; Gupta, V.; Yadav, T.P.; Gupta, V.; Singh, S.P. Green synthesis, characterization and antimicrobial activity of zinc oxide quantum dots using Eclipta alba. Mater. Chem. Phys. 2018, 203, 40–48. [Google Scholar] [CrossRef]
- Gupta, M.; Tomar, R.S.; Kaushik, S.; Mishra, R.K.; Sharma, D. Effective antimicrobial activity of green ZnO nano particles of Catharanthus roseus. Front. Microbiol. 2018, 9, 2030. [Google Scholar] [CrossRef]
- Aminuzzaman, M.; Ying, L.P.; Goh, W.S.; Watanabe, A. Green synthesis of zinc oxide nanoparticles using aqueous extract of Garcinia mangostana fruit pericarp and their photocatalytic activity. Bull. Mater. Sci. 2018, 41, 50. [Google Scholar] [CrossRef] [Green Version]
- Sharmila, G.; Thirumarimurugan, M.; Muthukumaran, C. Green synthesis of ZnO nanoparticles using Tecoma castanifolia leaf extract: Characterization and evaluation of its antioxidant, bactericidal and anticancer activities. Microchem. J. 2019, 145, 578–587. [Google Scholar] [CrossRef]
- Zhang, H.; Shan, Y.; Dong, L. A Comparison of TiO2 and ZnO Nanoparticles as Photosensitizers in Photodynamic Therapy for Cancer. J. Biomed. Nanotechnol. 2014, 10, 1450–1457. [Google Scholar] [CrossRef]
- Raheem, M.A.; Rahim, M.A.; Gul, I.; Zhong, X.; Xiao, C.; Zhang, H.; Wei, J.; He, Q.; Hassan, M.; Zhang, C.Y.; et al. Advances in nanoparticles-based approaches in cancer theranostics. OpenNano 2023, 12, 100152. [Google Scholar] [CrossRef]
- Faisal, S.; Jan, H.; Shah, S.A.; Shah, S.; Khan, A.; Akbar, M.T.; Rizwan, M.; Jan, F.; Wajidullah; Akhtar, N.; et al. Green Synthesis of Zinc Oxide (ZnO) Nanoparticles Using Aqueous Fruit Extracts of Myristica fragrans: Their Characterizations and Biological and Environmental Applications. ACS Omega 2021, 6, 9709–9722. [Google Scholar] [CrossRef] [PubMed]
- Naseer, M.; Aslam, U.; Khalid, B.; Chen, B. Green route to synthesize Zinc Oxide Nanoparticles using leaf extracts of Cassia fistula and Melia azadarach and their antibacterial potential. Sci. Rep. 2020, 10, 9055. [Google Scholar] [CrossRef]
- Iqbal, J.; Abbasi, B.A.; Yaseen, T.; Zahra, S.A.; Shahbaz, A.; Shah, S.A.; Uddin, S.; Ma, X.; Raouf, B.; Kanwal, S.; et al. Green synthesis of zinc oxide nanoparticles using Elaeagnus angustifolia L. leaf extracts and their multiple in vitro biological applications. Sci. Rep. 2021, 11, 20988. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, B.A.; Iqbal, J.; Ahmad, R.; Zia, L.; Kanwal, S.; Mahmood, T.; Wang, C.; Chen, J.T. Bioactivities of geranium wallichianum leaf extracts conjugated with zinc oxide nanoparticles. Biomolecules 2020, 10, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lingaraju, K.; Naika, H.R.; Nagabhushana, H.; Nagaraju, G. Euphorbia heterophylla (L.) mediated fabrication of ZnO NPs: Characterization and evaluation of antibacterial and anticancer properties. Biocatal. Agric. Biotechnol. 2019, 18, 100894. [Google Scholar] [CrossRef]
- Irfan, M.; Munir, H.; Ismail, H. Moringa oleifera gum based silver and zinc oxide nanoparticles: Green synthesis, characterization and their antibacterial potential against MRSA. Biomater. Res. 2021, 25, 17. [Google Scholar] [CrossRef]
- Madan, H.R.; Sharma, S.C.; Udayabhanu; Suresh, D.; Vidya, Y.S.; Nagabhushana, H.; Rajanaik, H.; Anantharaju, K.S.; Prashantha, S.C.; Sadananda Maiya, P. Facile green fabrication of nanostructure ZnO plates, bullets, flower, prismatic tip, closed pine cone: Their antibacterial, antioxidant, photoluminescent and photocatalytic properties. Spectrochim. Acta-Part A Mol. Biomol. Spectrosc. 2016, 152, 404–416. [Google Scholar] [CrossRef]
- Elumalai, K.; Velmurugan, S. Green synthesis, characterization and antimicrobial activities of zinc oxide nanoparticles from the leaf extract of Azadirachta indica (L.). Appl. Surf. Sci. 2015, 345, 329–336. [Google Scholar] [CrossRef]
- Thema, F.T.; Manikandan, E.; Dhlamini, M.S.; Maaza, M. Green synthesis of ZnO nanoparticles via Agathosma betulina natural extract. Mater. Lett. 2015, 161, 124–127. [Google Scholar] [CrossRef]
- Krupa, A.N.D.; Vimala, R. Evaluation of tetraethoxysilane (TEOS) sol-gel coatings, modified with green synthesized zinc oxide nanoparticles for combating microfouling. Mater. Sci. Eng. C 2016, 61, 728–735. [Google Scholar] [CrossRef] [PubMed]
- Sundrarajan, M.; Ambika, S.; Bharathi, K. Plant-extract mediated synthesis of ZnO nanoparticles using Pongamia pinnata and their activity against pathogenic bacteria. Adv. Powder Technol. 2015, 26, 1294–1299. [Google Scholar] [CrossRef]
- Ramesh, M.; Anbuvannan, M.; Viruthagiri, G. Green synthesis of ZnO nanoparticles using Solanum nigrum leaf extract and their antibacterial activity. Spectrochim. Acta-Part A Mol. Biomol. Spectrosc. 2015, 136, 864–870. [Google Scholar] [CrossRef] [PubMed]
- Fu, L.; Fu, Z. Plectranthus amboinicus leaf extract-assisted biosynthesis of ZnO nanoparticles and their photocatalytic activity. Ceram. Int. 2015, 41, 2492–2496. [Google Scholar] [CrossRef]
- Anbuvannan, M.; Ramesh, M.; Viruthagiri, G.; Shanmugam, N.; Kannadasan, N. Anisochilus carnosus leaf extract mediated synthesis of zinc oxide nanoparticles for antibacterial and photocatalytic activities. Mater. Sci. Semicond. Process. 2015, 39, 621–628. [Google Scholar] [CrossRef]
- Yuvakkumar, R.; Suresh, J.; Nathanael, A.J.; Sundrarajan, M.; Hong, S.I. Novel green synthetic strategy to prepare ZnO nanocrystals using rambutan (Nephelium lappaceum L.) peel extract and its antibacterial applications. Mater. Sci. Eng. C 2014, 41, 17–27. [Google Scholar] [CrossRef]
- Anbuvannan, M.; Ramesh, M.; Viruthagiri, G.; Shanmugam, N.; Kannadasan, N. Synthesis, characterization and photocatalytic activity of ZnO nanoparticles prepared by biological method. Spectrochim. Acta-Part A Mol. Biomol. Spectrosc. 2015, 143, 304–308. [Google Scholar] [CrossRef]
- Dobrucka, R.; Długaszewska, J. Biosynthesis and antibacterial activity of ZnO nanoparticles using Trifolium pratense flower extract. Saudi J. Biol. Sci. 2016, 23, 517–523. [Google Scholar] [CrossRef] [Green Version]
- Qian, Y.; Yao, J.; Russel, M.; Chen, K.; Wang, X. Characterization of green synthesized nano-formulation (ZnO-A. vera) and their antibacterial activity against pathogens. Environ. Toxicol. Pharmacol. 2015, 39, 736–746. [Google Scholar] [CrossRef]
- Husain, S.; Verma, S.K.; Yasin, D.; Hemlata; Rizvi, M.M.A.; Fatma, T. Facile green bio-fabricated silver nanoparticles from Microchaete infer dose-dependent antioxidant and anti-proliferative activity to mediate cellular apoptosis. Bioorg. Chem. 2021, 107, 104535. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.K.; Jha, E.; Sahoo, B.; Panda, P.K.; Thirumurugan, A.; Parashar, S.K.S.; Suar, M. Mechanistic insight into the rapid one-step facile biofabrication of antibacterial silver nanoparticles from bacterial release and their biogenicity and concentration-dependent in vitro cytotoxicity to colon cells. RSC Adv. 2017, 7, 40034–40045. [Google Scholar] [CrossRef] [Green Version]
- Moghaddam, A.B.; Moniri, M.; Azizi, S.; Rahim, R.A.; Ariff, A.B.; Saad, W.Z.; Namvar, F.; Navaderi, M.; Mohamad, R. Biosynthesis of ZnO nanoparticles by a new Pichia kudriavzevii yeast strain and evaluation of their antimicrobial and antioxidant activities. Molecules 2017, 22, 872. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eram, R.; Kumari, P.; Panda, P.; Singh, S.; Sarkar, B.; Mallick, M.; Verma, S. Cellular Investigations on Mechanistic Biocompatibility of Green Synthesized Calcium Oxide Nanoparticles with Danio rerio. J. Nanotheranostics 2021, 2, 51–62. [Google Scholar] [CrossRef]
- Amith Yadav, H.J.; Eraiah, B.; Nagabhushana, H.; Daruka Prasad, B.; Basavaraj, R.B.; Sateesh, M.K.; Shabaaz Begum, J.P.; Darshan, G.P.; Vijayakumar, G.R. Broad spectral inhibitory effects of pale green zinc oxide nanophosphor on bacterial and fungal pathogens. Arab. J. Chem. 2018, 11, 324–342. [Google Scholar] [CrossRef]
- Blecher, K.; Nasir, A.; Friedman, A. The growing role of nanotechnology in combating infectious disease. Virulence 2011, 2, 395–401. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morimoto, Y.; Izumi, H.; Yoshiura, Y.; Tomonaga, T.; Oyabu, T.; Myojo, T.; Kawai, K.; Yatera, K.; Shimada, M.; Kubo, M.; et al. Evaluation of pulmonary toxicity of zinc oxide nanoparticles following inhalation and intratracheal instillation. Int. J. Mol. Sci. 2016, 17, 1241. [Google Scholar] [CrossRef]
- Vimercati, L.; Cavone, D.; Caputi, A.; De Maria, L.; Tria, M.; Prato, E.; Ferri, G.M. Nanoparticles: An Experimental Study of Zinc Nanoparticles Toxicity on Marine Crustaceans. General Overview on the Health Implications in Humans. Front. Public Health 2020, 8, 192. [Google Scholar] [CrossRef]
- Skibba, M.; Drelich, A.; Poellmann, M.; Hong, S.; Brasier, A.R. Nanoapproaches to Modifying Epigenetics of Epithelial Mesenchymal Transition for Treatment of Pulmonary Fibrosis. Front. Pharmacol. 2020, 11, 607689. [Google Scholar] [CrossRef]
- Sharma, M.; Nikota, J.; Halappanavar, S.; Castranova, V.; Rothen-Rutishauser, B.; Clippinger, A.J. Predicting pulmonary fibrosis in humans after exposure to multi-walled carbon nanotubes (MWCNTs). Arch. Toxicol. 2016, 90, 1605–1622. [Google Scholar] [CrossRef]
- Sruthi, S.; Ashtami, J.; Mohanan, P.V. Biomedical application and hidden toxicity of Zinc oxide nanoparticles. Mater. Today Chem. 2018, 10, 175–186. [Google Scholar] [CrossRef]
- Choudhury, A.; Simnani, F.Z.; Singh, D.; Patel, P.; Sinha, A.; Nandi, A.; Ghosh, A.; Saha, U.; Kumari, K.; Jaganathan, S.K.; et al. Atmospheric microplastic and nanoplastic: The toxicological paradigm on the cellular system. Ecotoxicol. Environ. Saf. 2023, 259, 115018. [Google Scholar] [CrossRef]
- Scherzad, A.; Meyer, T.; Kleinsasser, N.; Hackenberg, S. Molecular Mechanisms of Zinc Oxide Nanoparticle-Induced Genotoxicity. Materials 2017, 10, 1427. [Google Scholar] [CrossRef] [Green Version]
- Tripathy, N.; Hong, T.-K.; Ha, K.-T.; Jeong, H.-S.; Hahn, Y.-B. Effect of ZnO nanoparticles aggregation on the toxicity in RAW 264.7 murine macrophage. J. Hazard. Mater. 2014, 270, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Manke, A.; Wang, L.; Rojanasakul, Y. Mechanisms of Nanoparticle-Induced Oxidative Stress and Toxicity. Biomed. Res. Int. 2013, 2013, 942916. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng, K.W.; Khoo, S.P.K.; Heng, B.C.; Setyawati, M.I.; Tan, E.C.; Zhao, X.; Xiong, S.; Fang, W.; Leong, D.T.; Loo, J.S.C. The role of the tumor suppressor p53 pathway in the cellular DNA damage response to zinc oxide nanoparticles. Biomaterials 2011, 32, 8218–8225. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, J.W.; Martinez, E.; Louka, P.; Wingett, D.G. Zinc oxide nanoparticles for selective destruction of tumor cells and potential for drug delivery applications. Expert Opin. Drug Deliv. 2010, 7, 1063–1077. [Google Scholar] [CrossRef] [Green Version]
- Długosz, O.; Szostak, K.; Staroń, A.; Pulit-Prociak, J.; Banach, M. Methods for Reducing the Toxicity of Metal and Metal Oxide NPs as Biomedicine. Materials 2020, 13, 279. [Google Scholar] [CrossRef] [Green Version]
- AshaRani, P.V.; Low Kah Mun, G.; Hande, M.P.; Valiyaveettil, S. Cytotoxicity and Genotoxicity of Silver Nanoparticles in Human Cells. ACS Nano 2009, 3, 279–290. [Google Scholar] [CrossRef]
- de Lima, R.; Seabra, A.B.; Durán, N. Silver nanoparticles: A brief review of cytotoxicity and genotoxicity of chemically and biogenically synthesized nanoparticles. J. Appl. Toxicol. 2012, 32, 867–879. [Google Scholar] [CrossRef]
- Alavi, N.; Maghami, P.; Fani Pakdel, A.; Rezaei, M.; Avan, A. The advance anticancer role of polymeric core-shell ZnO nanoparticles containing oxaliplatin in colorectal cancer. J. Biochem. Mol. Toxicol. 2023, 37, e23325. [Google Scholar] [CrossRef] [PubMed]
- Si, B.; Song, E. Recent Advances in the Detection of Neurotransmitters. Chemosensors 2018, 6, 1. [Google Scholar] [CrossRef] [Green Version]
- Mueller, N.C.; Nowack, B. Nanoparticles for Remediation: Solving Big Problems with Little Particles. Elements 2010, 6, 395–400. [Google Scholar] [CrossRef]
- Shrivastava, R.; Raza, S.; Yadav, A.; Kushwaha, P.; Flora, S.J.S. Effects of sub-acute exposure to TiO2, ZnO and Al2O3 nanoparticles on oxidative stress and histological changes in mouse liver and brain. Drug Chem. Toxicol. 2014, 37, 336–347. [Google Scholar] [CrossRef]
- Salehi, H.; Chehregani Rad, A.; Sharifan, H.; Raza, A.; Varshney, R.K. Aerially Applied Zinc Oxide Nanoparticle Affects Reproductive Components and Seed Quality in Fully Grown Bean Plants (Phaseolus vulgaris L.). Front. Plant Sci. 2022, 12, 808141. [Google Scholar] [CrossRef]
- Dianová, L.; Tirpák, F.; Halo, M.; Slanina, T.; Massányi, M.; Stawarz, R.; Formicki, G.; Madeddu, R.; Massányi, P. Effects of Selected Metal Nanoparticles (Ag, ZnO, TiO2) on the Structure and Function of Reproductive Organs. Toxics 2022, 10, 459. [Google Scholar] [CrossRef]
- Torabi, F.; Shafaroudi, M.M.; Rezaei, N. Combined protective effect of zinc oxide nanoparticles and melatonin on cyclophosphamide-induced toxicity in testicular histology and sperm parameters in adult Wistar rats. Int. J. Reprod. Biomed. 2017, 15, 403–412. [Google Scholar] [CrossRef] [Green Version]
- Teng, C.; Jia, J.; Wang, Z.; Sharma, V.K.; Yan, B. Size-dependent maternal-fetal transfer and fetal developmental toxicity of ZnO nanoparticles after oral exposures in pregnant mice. Ecotoxicol. Environ. Saf. 2019, 182, 109439. [Google Scholar] [CrossRef]
- An, S.S.A.; Hong, J.-S.; Park, M.-K.; Kim, M.-S.; Lim, J.-H.; Park, G.-J.; Meang, E.-H.; Jeong, J.; Shin, J.-H.; Kim, M.-K.; et al. Prenatal development toxicity study of zinc oxide nanoparticles in rats. Int. J. Nanomed. 2014, 9, 159–171. [Google Scholar] [CrossRef] [Green Version]
- Panda, P.K.; Verma, S.K.; Suar, M. Nanoparticle-biological interactions: The renaissance of bionomics in the myriad nanomedical technologies. Nanomedicine 2021, 16, 2249–2254. [Google Scholar] [CrossRef]
- Chang, Y.N.; Zhang, M.; Xia, L.; Zhang, J.; Xing, G. The toxic effects and mechanisms of CuO and ZnO nanoparticles. Materials 2012, 5, 2850–2871. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.; Yu, W.J.; Song, J.; Sung, C.; Jeong, E.J.; Han, J.S.; Kim, P.; Jo, E.; Eom, I.; Kim, H.M.; et al. Developmental toxicity of intravenously injected zinc oxide nanoparticles in rats. Arch. Pharm. Res. 2016, 39, 1682–1692. [Google Scholar] [CrossRef] [PubMed]
- Babaie, S.; Taghvimi, A.; Hong, J.H.; Hamishehkar, H.; An, S.; Kim, K.H. Recent advances in pain management based on nanoparticle technologies. J. Nanobiotechnol. 2022, 20, 290. [Google Scholar] [CrossRef]
- Chen, Y.Y.; Lee, Y.H.; Wang, B.J.; Chen, R.J.; Wang, Y.J. Skin damage induced by zinc oxide nanoparticles combined with UVB is mediated by activating cell pyroptosis via the NLRP3 inflammasome–autophagy–exosomal pathway. Part. Fibre Toxicol. 2022, 19, 2. [Google Scholar] [CrossRef] [PubMed]
- Mohanty, S.; Patel, P.; Jha, E.; Panda, P.K.; Kumari, P.; Singh, S.; Sinha, A.; Saha, A.K.; Kaushik, N.K.; Raina, V.; et al. In vivo intrinsic atomic interaction infer molecular eco-toxicity of industrial TiO2 nanoparticles via oxidative stress channelized steatosis and apoptosis in Paramecium caudatum. Ecotoxicol. Environ. Saf. 2022, 241, 113708. [Google Scholar] [CrossRef]
- Sharma, S.V.; Bell, D.W.; Settleman, J.; Haber, D.A. Epidermal growth factor receptor mutations in lung cancer. Nat. Rev. Cancer 2007, 7, 169–181. [Google Scholar] [CrossRef]
- Gazdar, A.; Brambilla, E. Pathogenesis of Lung Cancer Signalling Pathways: Roadmap for Therapies. Eur. Respir J. 2019, 33, 1485–1497. [Google Scholar]
- Seshacharyulu, P.; Ponnusamy, M.P.; Haridas, D.; Jain, M.; Ganti, A.K.; Batra, S.K. Targeting the EGFR signaling pathway in cancer therapy. Expert Opin. Ther. Targets 2012, 16, 15–31. [Google Scholar] [CrossRef] [Green Version]
- Prior, I.A.; Lewis, P.D.; Mattos, C. A comprehensive survey of ras mutations in cancer. Cancer Res. 2012, 72, 2457–2467. [Google Scholar] [CrossRef] [Green Version]
- Lito, P.; Rosen, N.; Solit, D.B. Tumor adaptation and resistance to RAF inhibitors. Nat. Med. 2013, 19, 1401–1409. [Google Scholar] [CrossRef]
- Hatzivassiliou, G.; Haling, J.R.; Chen, H.; Song, K.; Price, S.; Heald, R.; Hewitt, J.F.M.; Zak, M.; Peck, A.; Orr, C.; et al. Mechanism of MEK inhibition determines efficacy in mutant KRAS- versus BRAF-driven cancers. Nature 2013, 501, 232–236. [Google Scholar] [CrossRef] [PubMed]
- Westcott, P.M.K.; To, M.D. The genetics and biology of KRAS in lung cancer. Chin. J. Cancer 2013, 32, 63–70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, Z.; Golay, H.G.; Barbie, D.A. Targeting pathways downstream of KRAS in lung adenocarcinoma. Pharmacogenomics 2014, 15, 1507–1518. [Google Scholar] [CrossRef] [Green Version]
- Nau, M.M.; Brooks, B.J.; Battey, J.; Sausville, E.; Gazdar, A.F.; Kirsch, I.R.; McBride, O.W.; Bertness, V.; Hollis, G.F.; Minna, J.D. L-myc, a new myc-related gene amplified and expressed in human small cell lung cancer. Nature 1985, 318, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Massague, J. TGFbeta in Cancer. Cell 2008, 134, 215–230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akhurst, R.J.; Hata, A. Targeting the TGFβ signalling pathway in disease. Nat. Rev. Drug Discov. 2012, 11, 790–811. [Google Scholar] [CrossRef] [Green Version]
- Derynck, R.; Zhang, Y.E. Smad-dependent and Smad-independent pathways in TGF-β family signalling. Nature 2003, 425, 577–584. [Google Scholar] [CrossRef]
- Clevers, H.; Nusse, R. Wnt/β-catenin signaling and disease. Cell 2012, 149, 1192–1205. [Google Scholar] [CrossRef] [Green Version]
- Anastas, J.N.; Moon, R.T. WNT signalling pathways as therapeutic targets in cancer. Nat. Rev. Cancer 2013, 13, 11–26. [Google Scholar] [CrossRef]
- Fong, K.M.; Sekido, Y.; Minna, J.D. Molecular pathogenesis of lung cancer. J. Thorac. Cardiovasc. Surg. 1999, 118, 1136–1152. [Google Scholar] [CrossRef] [Green Version]
- Jones, P.A.; Baylin, S.B. The fundamental role of epigenetic events in cancer. Nat. Rev. Genet. 2002, 3, 415–428. [Google Scholar] [CrossRef] [PubMed]
- Epigenetics, C.; Mechanism, F. Cancer Epigenetics: From Mechanism to Therapy. Cell 2012, 150, 12–27. [Google Scholar]
- Chi, P.; Allis, C.D.; Wang, G.G. Covalent histone modifications—Miswritten, misinterpreted and mis-erased in human cancers. Nat. Rev. Cancer 2010, 10, 457–469. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanahan, D.; Folkman, J. Patterns and emerging mechanisms of the angiogenic switch during tumorigenesis. Cell 1996, 86, 353–364. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aggarwal, V.; Tuli, H.; Varol, A.; Thakral, F.; Yerer, M.; Sak, K.; Varol, M.; Jain, A.; Khan, M.; Sethi, G. Role of Reactive Oxygen Species in Cancer Progression: Molecular Mechanisms and Recent Advancements. Biomolecules 2019, 9, 735. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Godoy-Gallardo, M.; Eckhard, U.; Delgado, L.M.; de Roo Puente, Y.J.D.; Hoyos-Nogués, M.; Gil, F.J.; Perez, R.A. Antibacterial approaches in tissue engineering using metal ions and nanoparticles: From mechanisms to applications. Bioact. Mater. 2021, 6, 4470–4490. [Google Scholar] [CrossRef]
- Zhang, T.; Du, E.; Liu, Y.; Cheng, J.; Zhang, Z.; Xu, Y.; Qi, S.; Chen, Y. Anticancer Effects of Zinc Oxide Nanoparticles Through Altering the Methylation Status of Histone on Bladder Cancer Cells. Int. J. Nanomed. 2020, 15, 1457–1468. [Google Scholar] [CrossRef] [Green Version]
- Sayed, H.M.; Said, M.M.; Morcos, N.Y.S.; El Gawish, M.A.; Ismail, A.F.M. Antitumor and Radiosensitizing Effects of Zinc Oxide-Caffeic Acid Nanoparticles against Solid Ehrlich Carcinoma in Female Mice. Integr. Cancer Ther. 2021, 20, 153473542110219. [Google Scholar] [CrossRef]
- Liu, Y.; Zhou, J.; Li, Q.; Li, L.; Jia, Y.; Geng, F.; Zhou, J.; Yin, T. Tumor microenvironment remodeling-based penetration strategies to amplify nanodrug accessibility to tumor parenchyma. Adv. Drug Deliv. Rev. 2021, 172, 80–103. [Google Scholar] [CrossRef]
- Patrón-Romero, L.; Luque-Morales, P.A.; Loera-Castañeda, V.; Lares-Asseff, I.; Leal-Ávila, M.Á.; Alvelais-Palacios, J.A.; Plasencia-López, I.; Almanza-Reyes, H. Mitochondrial Dysfunction Induced by Zinc Oxide Nanoparticles. Crystals 2022, 12, 1089. [Google Scholar] [CrossRef]
- Guo, Y.J.; Muharnmad, F.; Guo, M.Y.; Qi, W.X.; Sun, F.X.; Wang, A.F.; Zhu, G.S. pH-Triggered Controlled Drug Release from Mesoporous Silica Nanoparticles via Intracelluar Dissolution of ZnO Nanolids. J. Am. Chem. Soc. 2011, 133, 8778–8781. [Google Scholar]
- Mitra, S.B.S.; Patra, P.; Chandra, S.; Debnath, N.; Das, S.; Banerjee, R.; Kundu, S.C.; Pramanik, P.; Goswami, A. Porous ZnO nanorod for targeted delivery of doxorubicin: In vitro and in vivo response for therapeutic applications. J. Mater. Chem. 2012, 22, 24145–24154. [Google Scholar] [CrossRef]
- Zhang, Z.-Y.; Xu, Y.-D.; Ma, Y.-Y.; Qiu, L.-L.; Wang, Y.; Kong, J.-L.; Xiong, H.-M. Biodegradable ZnO@polymer Core-Shell Nanocarriers: pH-Triggered Release of Doxorubicin In Vitro. Angew. Chemie 2013, 125, 4221–4225. [Google Scholar] [CrossRef]
- Tan, L.; Liu, J.; Zhou, W.; Wei, J.; Peng, Z. A novel thermal and pH responsive drug delivery system based on ZnO@PNIPAM hybrid nanoparticles. Mater. Sci. Eng. C 2014, 45, 524–529. [Google Scholar] [CrossRef]
- Zhu, J.; Niu, Y.; Li, Y.; Gong, Y.; Shi, H.; Huo, Q.; Liu, Y.; Xu, Q. Stimuli-responsive delivery vehicles based on mesoporous silica nanoparticles: Recent advances and challenges. J. Mater. Chem. B 2017, 5, 1339–1352. [Google Scholar] [CrossRef]
- Wang, Y.; Song, S.; Liu, J.; Liu, D.; Zhang, H. ZnO-Functionalized Upconverting Nanotheranostic Agent: Multi-Modality Imaging-Guided Chemotherapy with On-Demand Drug Release Triggered by pH. Angew. Chemie 2015, 127, 546–550. [Google Scholar] [CrossRef]
- Cai, X.; Luo, Y.; Yan, H.; Du, D.; Lin, Y. PH-Responsive ZnO Nanocluster for Lung Cancer Chemotherapy. ACS Appl. Mater. Interfaces 2017, 9, 5739–5747. [Google Scholar] [CrossRef]
- Zarreen Simnani, F.; Singh, D.; Patel, P.; Choudhury, A.; Sinha, A.; Nandi, A.; Kumar Samal, S.; Verma, S.K.; Kumar Panda, P. Nanocarrier vaccine therapeutics for global infectious and chronic diseases. Mater. Today 2023, 66, 371–408. [Google Scholar] [CrossRef]
- Agarwal, H.; Shanmugam, V. A review on anti-inflammatory activity of green synthesized zinc oxide nanoparticle: Mechanism-based approach. Bioorg. Chem. 2020, 94, 103423. [Google Scholar] [CrossRef]
- Wang, H.; Zhou, Y.; Sun, Q.; Zhou, C.; Hu, S.; Lenahan, C.; Xu, W.; Deng, Y.; Li, G.; Tao, S. Update on Nanoparticle-Based Drug Delivery System for Anti-inflammatory Treatment. Front. Bioeng. Biotechnol. 2021, 9, 630352. [Google Scholar] [CrossRef]
- Raha, S.; Ahmaruzzaman, M. ZnO nanostructured materials and their potential applications: Progress, challenges and perspectives. Nanoscale Adv. 2022, 4, 1868–1925. [Google Scholar] [CrossRef]
- Mobarez, E.; Azoz, H.; Alkalamawy, N.; Nada, A.-F. Evaluation the Effectiveness of Green Zinc Oxide Nanoparticles on The Anti-Inflammatory Effect of Dexamethasone and Its Side Effects in Rats. SVU-Int. J. Vet. Sci. 2018, 1, 25–54. [Google Scholar] [CrossRef]
- Rahimi Kalateh Shah Mohammad, G.; Homayouni Tabrizi, M.; Ardalan, T.; Yadamani, S.; Safavi, E. Green synthesis of zinc oxide nanoparticles and evaluation of anti-angiogenesis, anti-inflammatory and cytotoxicity properties. J. Biosci. 2019, 44, 30. [Google Scholar] [CrossRef]
- Sarkar, K.; Dutta, K.; Chatterjee, A.; Sarkar, J.; Das, D.; Prasad, A.; Chattopadhyay, D.; Acharya, K.; Das, M.; Verma, S.K.; et al. Nanotherapeutic potential of antibacterial folic acid-functionalized nanoceria for wound-healing applications. Nanomedicine 2023, 18, 109–123. [Google Scholar] [CrossRef] [PubMed]
- Rahimi, G.; Mohammad, K.S.; Zarei, M.; Shokoohi, M.; Oskoueian, E.; Poorbagher, M.R.M.; Karimi, E. Zinc oxide nanoparticles synthesized using Hyssopus Officinalis L. Extract Induced oxidative stress and changes the expression of key genes involved in inflammatory and antioxidant Systems. Biol. Res. 2022, 55, 24. [Google Scholar] [CrossRef]





| Sl.No. | Drug | Cell Lines | Characteristics | References |
|---|---|---|---|---|
| 1. | Doxorubicin (DOX) | HeLa cell line | Utilizing ZnO nano lids initiates pH-responsive drug release from mesoporous silica nanoparticles (MSN), resulting in a synergistic anticancer effect. | [156] |
| 2. | Doxorubicin | MDA-MB-231 cell line | Porous ZnO nanorods functionalized with folic acid and loaded with DOX demonstrate targeted and pH-responsive drug release and increased cytotoxicity compared to free DOX. | [157] |
| 3. | Doxorubicin | Human glioblastoma (U251) cell line | Core-shell nano-carriers consisting of biodegradable ZnO@polymer demonstrate pH-dependent drug release and higher cytotoxicity compared to free DOX. | [158] |
| 4. | Doxorubicin | - | Nanohybrids of ZnO and poly(N-isopropylacrylamide) exhibit drug release responsive to changes in pH and temperature. | [159] |
| 5. | Doxorubicin | HepG2 cells | A drug delivery system (DDS) created on mesoporous silica nanoparticles (MSN) with charge-reversal properties and gated by ZnO quantum dots (QDs) demonstrates pH-dependent drug release. It produces a synergistic anticancer effect when loaded with Dox. | [160] |
| 6. | Doxorubicin | HeLa cell line | An upconverting nano theranostic agent functionalized with ZnO and loaded with DOX demonstrates pH-dependent drug release and produces higher cytotoxicity than free DOX. | [161] |
| 7. | Doxorubicin | A549 cells | DOX-loaded ZnO quantum dots (QDs) functionalized with hyaluronic acid demonstrate targeted and pH-responsive drug release, resulting in higher cytotoxicity than non-targeted nano-carriers. | [162] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naser, S.S.; Ghosh, B.; Simnani, F.Z.; Singh, D.; Choudhury, A.; Nandi, A.; Sinha, A.; Jha, E.; Panda, P.K.; Suar, M.; et al. Emerging Trends in the Application of Green Synthesized Biocompatible ZnO Nanoparticles for Translational Paradigm in Cancer Therapy. J. Nanotheranostics 2023, 4, 248-279. https://doi.org/10.3390/jnt4030012
Naser SS, Ghosh B, Simnani FZ, Singh D, Choudhury A, Nandi A, Sinha A, Jha E, Panda PK, Suar M, et al. Emerging Trends in the Application of Green Synthesized Biocompatible ZnO Nanoparticles for Translational Paradigm in Cancer Therapy. Journal of Nanotheranostics. 2023; 4(3):248-279. https://doi.org/10.3390/jnt4030012
Chicago/Turabian StyleNaser, Shaikh Sheeran, Basab Ghosh, Faizan Zarreen Simnani, Dibyangshee Singh, Anmol Choudhury, Aditya Nandi, Adrija Sinha, Ealisha Jha, Pritam Kumar Panda, Mrutyunjay Suar, and et al. 2023. "Emerging Trends in the Application of Green Synthesized Biocompatible ZnO Nanoparticles for Translational Paradigm in Cancer Therapy" Journal of Nanotheranostics 4, no. 3: 248-279. https://doi.org/10.3390/jnt4030012
APA StyleNaser, S. S., Ghosh, B., Simnani, F. Z., Singh, D., Choudhury, A., Nandi, A., Sinha, A., Jha, E., Panda, P. K., Suar, M., & Verma, S. K. (2023). Emerging Trends in the Application of Green Synthesized Biocompatible ZnO Nanoparticles for Translational Paradigm in Cancer Therapy. Journal of Nanotheranostics, 4(3), 248-279. https://doi.org/10.3390/jnt4030012