Advances in Epithelial-Mesenchymal Transition (EMT)
A topical collection in Cells (ISSN 2073-4409). This collection belongs to the section "Stem Cells".
Viewed by 5356Editors
Interests: stem cells; biomaterials; regenerative medicine
Special Issues, Collections and Topics in MDPI journals
Interests: regenerative medicine; stem cells; oral stem cells; biomaterials; extracellular vesicles; exosomes; epithelial- mesenchymal transition
Special Issues, Collections and Topics in MDPI journals
Interests: regenerative medicine; stem cells; biomaterials; extracellular vesicles; exosomes; cardiac regeneration; cardiomyocytes
Special Issues, Collections and Topics in MDPI journals
Interests: regenerative medicine; stem cells; microfluidics; oral stem cells; restorative dentistry; osteoregeneration; biomaterials; epithelial–mesenchymal transition; extracellular vesicles; exosomes; liposomes
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
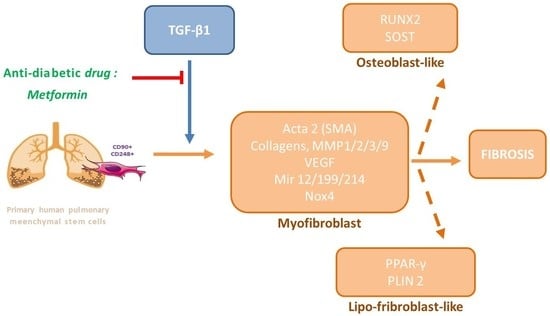
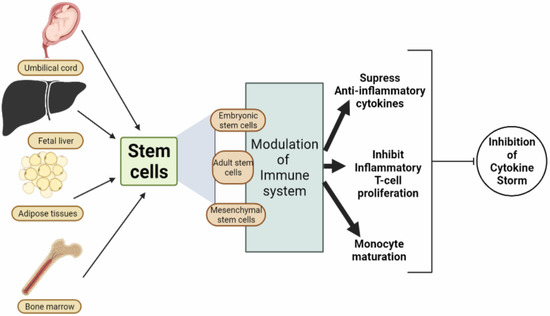
The epithelial–mesenchymal transition (EMT) is a process that leads to the transdifferentiation of epithelial cells into motile mesenchymal cells. This is an essential event in development, wound healing, and stem cell behaviour, and contributes pathologically to fibrosis and cancer progression.
The cell differentiation is regulated by several transcription factors and molecular mechanisms that still remain unknown. During EMT, cell–cell and cell–extracellular matrix interactions are remodelled, and a new transcriptional programme is activated to promote the modifications in cellular morphology and functions. We invite colleagues to contribute editorials, original research articles, or review papers with recent findings on the mechanisms and roles of EMT in normal and neoplastic tissues, during physiological and pathological processes.
Prof. Dr. Oriana Trubiani
Dr. Francesca Diomede
Dr. Jacopo Pizzicanella
Dr. Guya Marconi
Collection Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Cells is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2700 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- epithelial–mesenchymal transition
- fibrosis
- wound healing
- cancer
- development
- stem cell behaviour
- transcriptional factor
- cell differentiation