Atrial Fibrillation and Heart Failure
A special issue of Life (ISSN 2075-1729). This special issue belongs to the section "Medical Research".
Deadline for manuscript submissions: closed (30 November 2023) | Viewed by 17331
Special Issue Editors
Interests: catheter ablation; supraventricular tachycardia; atrial fibrillation; heart failure; ventricular tachycardia; pacemaker implantation
Special Issues, Collections and Topics in MDPI journals
Interests: atrial fibrillation; ventricular arrhythmia; PVC; ventricular tachycardia; supraventricular tachycardia; catheter ablation; cryoablation; heart failure; pediatric cardiology; cardiac resynchronization therapy
Special Issues, Collections and Topics in MDPI journals
Special Issue Information
Dear Colleagues,
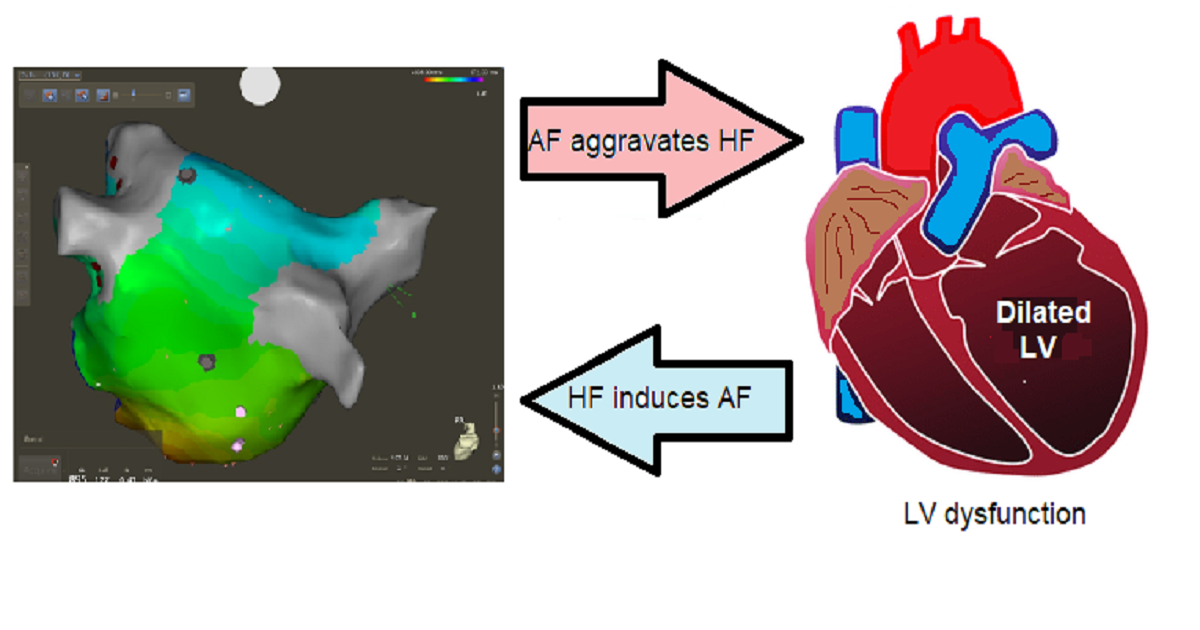
Many risk factors are shared by atrial fibrillation and heart failure, including hypertension, obesity, diabetes, and ischemic heart disease. This is why atrial fibrillation and heart failure are two clinical entities that can present alone but are frequently encountered together; it is not surprising for a patient to have both at the same time. Atrial fibrillation is currently the leading cause of ischemic stroke, as it causes blood clots at the level of the left atrial appendage or left atrium, which may break off and travel to the cerebral arteries. Heart failure can be caused by any condition that prevents the heart from pumping blood to the body or from completely filling the left ventricle, which is a feature of atrial fibrillation.
Pharmacological rhythm control is especially difficult in heart failure patients. Because of their negative inotropic effects, antiarrhythmic drugs such as flecainide and propafenone cannot be used. Amiodarone is the only AAD drug approved for HFrEF heart failure with a low ejection fraction, but it has a variety of side effects. As a result, rate versus rhythm strategies have been used to determine whether rhythm control is beneficial. If a person with AF does not respond to medication, or side effects occur, then catheter ablation may be necessary. Pulmonary vein isolation is considered the cornerstone of catheter ablation for AF because no other ablation options have shown benefit thus far.
However, there are still knowledge gaps in the appropriate management of patients with concomitant AF and HF: What is the best method to quantify atrial fibrosis in patients with heart failure? What is the optimal ablation strategy for persistent atrial fibrillation? What is the role of left atrial appendage occlusion or exclusion in patients with AF and HF? Is CRT implantation +AV node ablation superior to pulmonary vein isolation in patients with decreased LV ejection fraction and heart failure? In order for all of these questions to be answered, observational and prospective studies are expected in the near future.
For this Special Issue, we welcome original research, narrative review articles and meta-analyses on any topic related to atrial fibrillation and heart failure, from experimental research to epidemiological observations and therapeutic trials.
Topics relevant to this Special Issue include, but are not limited to:
- Experimental development of atrial fibrosis;
- Experimental induction of atrial fibrillation and heart failure in animals, and challenges in systemic thrombolysis;
- Observational studies on AF prevalence in the United States, Europe, Asia, Australia, Africa, and the Americas;
- Reviews on the pathophysiology and cellular basis of AF and HF;
- Arrhythmia-induced cardiomyopathy due to atrial fibrillation;
- Anticoagulation particularities in patients with AF and HF;
- Role of LA appendage exclusion and occlusion in AF and HF;
- Antiarrhythmic drugs for AF therapy in patients with HF;
- Reviews of catheter ablation trials versus medical treatment in AF with systolic dysfunction;
- Role of atrioventricular node ablation plus CRT in patients with AF and low ejection left ventricle.
Dr. Gabriel Cismaru
Dr. Alina Negru
Dr. Ernst R. Schwarz
Guest Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the special issue website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Life is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2600 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- atrial fibrillation
- heart failure
- stroke
- catheter ablation
- cardiac resynchronization therapy
- atrial fibrosis
- imaging
- antiarrhythmic drugs
Benefits of Publishing in a Special Issue
- Ease of navigation: Grouping papers by topic helps scholars navigate broad scope journals more efficiently.
- Greater discoverability: Special Issues support the reach and impact of scientific research. Articles in Special Issues are more discoverable and cited more frequently.
- Expansion of research network: Special Issues facilitate connections among authors, fostering scientific collaborations.
- External promotion: Articles in Special Issues are often promoted through the journal's social media, increasing their visibility.
- e-Book format: Special Issues with more than 10 articles can be published as dedicated e-books, ensuring wide and rapid dissemination.
Further information on MDPI's Special Issue polices can be found here.








