Advances in Neurodegenerative Diseases
A topical collection in Neurology International (ISSN 2035-8377).
Viewed by 72848Editors
2. School of Medicine, University of Thessaly, 41110 Larissa, Greece
Interests: neurosciences; neurology; neurogenetics; molecular neurology; neurodegeneration; neurorehabilitation
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
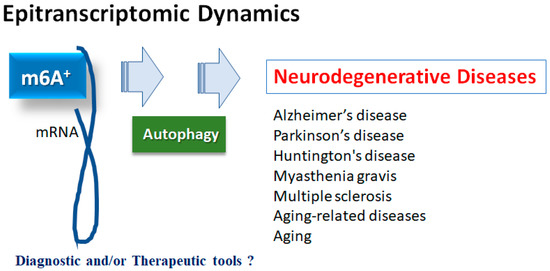
‘Neurodegeneration’ refers to a condition where neuronal cells slowly lose their functional potential and, ultimately, die. The term ‘neurodegenerative disorders’ is an umbrella term, encompassing a multitude of diseases that have a wide variety of phenotypes, depending on the neurons that degenerate each time. These various patterns of degeneration also stem from different pathophysiological mechanisms. For example, Alzheimer’s disease is characterized by the accumulation of pathologic amyloid and leads to dementia, while Parkinson’s disease is characterized by dopaminergic neuron loss, and predominantly leads to extrapyramidal symptoms. In principle, neurodegenerative disorders are particularly hard to tackle, and only symptomatic treatments are available—and not for all of the diseases. Considering they affect a significant proportion of the population, finding an effective treatment is crucial.
Neurodegenerative disorders have long captivated the interest of neuroscientists and significant advances in unraveling the mechanisms behind each neurodegenerative disorder have been noted. For instance, the role of the endoplasmic reticulum has slowly started being understood, and this can open up new therapeutic avenues. Furthermore, genetic components, epigenetic alterations, and environmental risk factors have been incriminated in their manifestation, and their combination can help identify individuals at risk. For instance, the deregulation of specific microRNA molecules can create a unique ‘signature’ for each disorder, and possibly lead to an earlier diagnosis. Therapy-wise, the optimizing of older symptomatic treatments has been fruitful in many cases, but disease-modifying therapies are still lacking and many are still under trial. These therapies include immunotherapies, enzyme inhibitors or activators, chaperone proteins, and antioxidative compounds, while gene treatments for hereditary disorders have also attracted attention. Finally, non-invasive brain stimulation also seems to hold much promise. As such, highlighting the newest research results and collecting the available evidence are now more important than ever.
This Topical Collection aims to cover the newest advancements in the field of neurodegeneration, and invites authors to contribute original studies, reviews, meta-analyses and related case reports regarding epidemiology, genetics, risk factors, diagnosis, management and prognosis assessment of neurodegenerative diseases. All article types are welcome.
Dr. Vasileios Siokas
Dr. Efthimios Dardiotis
Collection Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Neurology International is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 1600 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- neurodegenerative disorders
- Alzheimer’s disease
- Parkinson’s disease
- motor neuron disease
- neurodegeneration