Journal Description
Sinusitis
Sinusitis
(Volume 3, Issue 3 - 2018 was published with Sinusitis and Asthma) is a peer-reviewed, open access journal which focuses on medical research about sinusitis, and is published semiannually online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 22.6 days after submission; acceptance to publication is undertaken in 2.7 days (median values for papers published in this journal in the second half of 2024).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
- Sinusitis is a companion journal of JCM.
Latest Articles
The Impact of Churg–Strauss Syndrome on Nasal Function and Quality of Life: An Underexplored Dimension
Sinusitis 2025, 9(1), 3; https://doi.org/10.3390/sinusitis9010003 - 30 Jan 2025
Abstract
Eosinophilic Granulomatosis with Polyangiitis (EGPA)/Churg–Strauss syndrome is a systemic vasculitis that often causes chronic nasal dysfunction, including anosmia, nasal obstruction, and sinusitis. Anosmia, affecting up to 20% of EGPA patients, has a significant negative impact on quality of life (QoL). The loss of
[...] Read more.
Eosinophilic Granulomatosis with Polyangiitis (EGPA)/Churg–Strauss syndrome is a systemic vasculitis that often causes chronic nasal dysfunction, including anosmia, nasal obstruction, and sinusitis. Anosmia, affecting up to 20% of EGPA patients, has a significant negative impact on quality of life (QoL). The loss of smell disrupts daily activities, reduces enjoyment of food, and impairs social interactions, leading to feelings of isolation, depression, and anxiety. These psychosocial consequences, combined with persistent physical symptoms, contribute to a marked decline in overall well-being and are among the strongest predictors of poor QoL in EGPA patients. Early diagnosis and intervention are essential to mitigate these effects and improve patient outcomes. A multidisciplinary approach that combines pharmacological treatment, surgical options, and psychosocial support is critical to managing both the physical and emotional challenges of nasal dysfunction in EGPA. However, further research is needed to explore long-term management strategies, optimize therapeutic approaches, and better address the complex interplay between physical symptoms and QoL in EGPA patients.
Full article
Open AccessCase Report
Sinonasal Mass in the Setting of Prior Maxillofacial Surgery and Solid Organ Malignancy
by
Yihuai Qu, Jeffrey C. Mecham and Michael J. Marino
Sinusitis 2025, 9(1), 2; https://doi.org/10.3390/sinusitis9010002 - 25 Jan 2025
Abstract
►▼
Show Figures
Fungal rhinosinusitis (FRS) can be classified into invasive and non-invasive forms, with the fungal ball (FB) representing a common non-invasive type with generally favorable outcomes post-operatively. The clinical presentation of FB can vary and be non-specific, and it is important to consider a
[...] Read more.
Fungal rhinosinusitis (FRS) can be classified into invasive and non-invasive forms, with the fungal ball (FB) representing a common non-invasive type with generally favorable outcomes post-operatively. The clinical presentation of FB can vary and be non-specific, and it is important to consider a wide differential diagnosis for sinonasal masses, including malignancy. We present the case of a 74-year-old female presenting with a two-year history of nasal obstruction and drainage. She has a history of breast cancer and prior maxillomandibular surgery, and imaging showed a poorly defined mass in the right maxillary sinus with possible hemorrhagic and/or proteinaceous content. Rigid nasal endoscopy revealed a friable mass, and endoscopic sinus surgery findings were consistent with FB. This case exemplifies the need to consider a broad set of differential diagnoses when evaluating sinonasal masses, especially if the patient has a prior malignancy or maxillomandibular surgical history, including FB and metastases to the paranasal sinuses. Given the presence of non-specific symptoms, it is important to consider early imaging for patients with distorted anatomy and a history of malignancy. Endoscopic sinus surgery, with high success rates, is the gold-standard treatment for FB.
Full article

Figure 1
Open AccessCase Report
Odontogenic Sinusitis of Endodontic Origin: Successful Management Through Endodontic Treatment
by
Marcelo Rolla, Karem Paula Pinto, Luciana Moura Sassone and Emmanuel João Nogueira Leal Silva
Sinusitis 2025, 9(1), 1; https://doi.org/10.3390/sinusitis9010001 - 9 Jan 2025
Abstract
►▼
Show Figures
Odontogenic sinusitis is a maxillary sinus infection arising from dental pathology, primarily involving posterior maxillary teeth due to their anatomical proximity to the sinus floor. Endodontic infections are a significant etiological factor, yet the condition is frequently underdiagnosed due to its overlapping presentation
[...] Read more.
Odontogenic sinusitis is a maxillary sinus infection arising from dental pathology, primarily involving posterior maxillary teeth due to their anatomical proximity to the sinus floor. Endodontic infections are a significant etiological factor, yet the condition is frequently underdiagnosed due to its overlapping presentation with sinonasal sinusitis. The present cases illustrate the diagnosis, management, and outcomes of maxillary sinusitis of endodontic origin through endodontic interventions. Two patients with histories of recurrent maxillary sinusitis underwent dental evaluations after conventional medical therapies failed. Cone-beam computed tomography confirmed the dental etiology in all cases, identifying inadequately treated second mesiobuccal (MB2) canals or significant periapical pathology. Endodontic retreatments were employed to address the underlying dental causes, followed by resolution of sinus symptoms within days. Follow-up imaging demonstrated ongoing bone healing and resolution of sinus involvement. These cases underscore the importance of addressing the dental etiology in maxillary sinusitis of endodontic origin to achieve complete symptom resolution and minimize recurrence. Cone-beam computed tomography proved instrumental in diagnosing and planning treatment, enabling precise management of periapical and sinus conditions. The cases highlight the necessity of a multidisciplinary approach, involving dental and medical professionals, to optimize outcomes.
Full article

Figure 1
Open AccessCase Report
A Single-Stage Procedure for Correction of Silent Sinus Syndrome: A Case Report About Our Experience
by
Aurelio D’Ecclesia, Stefano Patruno, Christian Fiorentino and Lazzaro Cassano
Sinusitis 2024, 8(2), 68-71; https://doi.org/10.3390/sinusitis8020009 - 3 Dec 2024
Abstract
►▼
Show Figures
Silent sinus syndrome is a rare condition characterized by an almost always unilateral collapse of the maxillary sinus. The most characteristic symptom of this syndrome is enophthalmos. Naso-sinusal disorders are rarely associated with this condition. We are going to discuss a case that
[...] Read more.
Silent sinus syndrome is a rare condition characterized by an almost always unilateral collapse of the maxillary sinus. The most characteristic symptom of this syndrome is enophthalmos. Naso-sinusal disorders are rarely associated with this condition. We are going to discuss a case that was associated with recurrent sinusitis. In this case report, we describe how we managed this rare syndrome so we can share our experience with those colleagues that may face this condition.
Full article

Figure 1
Open AccessCase Report
Recurrent Nasal Polyposis and Bifid Epiglottis in a Child with Bardet–Biedl Syndrome Ciliopathy
by
Natalia Fourla, Nikolaos Drimalas and Ioannis Michael Vlastos
Sinusitis 2024, 8(2), 63-67; https://doi.org/10.3390/sinusitis8020008 - 14 Nov 2024
Abstract
►▼
Show Figures
Bardet–Biedl syndrome (BBS) is a genetic disease caused by mutations of the BBS genes that encode proteins involved in cilia functioning. It can present with major and/or minor clinical manifestations, such as rod–cone dystrophy, polydactyly, obesity, speech delay, anosmia, congenital heart disease and
[...] Read more.
Bardet–Biedl syndrome (BBS) is a genetic disease caused by mutations of the BBS genes that encode proteins involved in cilia functioning. It can present with major and/or minor clinical manifestations, such as rod–cone dystrophy, polydactyly, obesity, speech delay, anosmia, congenital heart disease and genital and renal abnormalities. Diagnosis of this rare disease is based on clinical criteria and can be confirmed with molecular genetic testing. Although BBS is a ciliopathy, nasal polyposis has never before been reported in patients with this condition. This article presents the case of a 12-year-old male patient admitted with symptoms of retinopathy, development delay, anosmia, bifid epiglottis and recurrent nasal polyposis. After several clinical, imaging and genetic examinations, the patient was diagnosed with BBS. His nasal symptoms were treated with functional endoscopic sinus surgery and long-term antibiotic therapy, whereas courses of topical antibiotics as well as topical and systemic corticosteroids had no effect. As a conclusion, it is a rare case that presents new clinical manifestations (nasal polyps) that can be related to BBS and possible effective treatments.
Full article

Figure 1
Open AccessSystematic Review
The Association of Sinusitis with Central Skull Base Osteomyelitis: A Systematic Review
by
Owen Tsung Wen Ho and Alex Chengyao Tham
Sinusitis 2024, 8(2), 51-62; https://doi.org/10.3390/sinusitis8020007 - 30 Oct 2024
Abstract
►▼
Show Figures
We aim to provide an updated and comprehensive review of the current literature on the clinical profile and treatment options of CSBO caused by sinusitis. Three databases, Pubmed, Embase and Scopus, were searched from inception until 2 October 2022. Titles and abstracts were
[...] Read more.
We aim to provide an updated and comprehensive review of the current literature on the clinical profile and treatment options of CSBO caused by sinusitis. Three databases, Pubmed, Embase and Scopus, were searched from inception until 2 October 2022. Titles and abstracts were used for the first stage of study selection; subsequently, full texts were screened for final inclusion. Nine studies were included, with eight case reports and one case series. Patients ranged between 33 and 75 years old, with four females and four males total in the case reports. In the case series, there were 14 patients with a mean age of 62 years old. Patients with CSBO secondary to sinusitis often present with non-specific symptoms which may mimic other pathologies of the head and neck. A high index of suspicion for CSBO is important in the presence of an unremitting headache or cranial nerve palsy. Treatment options include culture-directed long-term antibiotics and surgery. The role of surgery in these patients, however, needs to be investigated more thoroughly. We believe that more large-cohort observational studies assessing the association between sinusitis and CSBO should be performed to further analyze and evaluate this topic.
Full article

Figure 1
Open AccessReview
What We Know about Nasal Polyposis: The Clinician’s Point of View
by
Philippe Eloy and Gabriela Cornelia Musat
Sinusitis 2024, 8(2), 37-50; https://doi.org/10.3390/sinusitis8020006 - 26 Sep 2024
Abstract
►▼
Show Figures
Nasal polyposis is defined as a Th2-driven chronic inflammation of the nose and sinus with polyps visible in the nasal fossae. It is a prevalent disease with a significant impact on health-related quality of life (HRQL). Allergies, allergic rhinitis, asthma, and aspirin intolerance
[...] Read more.
Nasal polyposis is defined as a Th2-driven chronic inflammation of the nose and sinus with polyps visible in the nasal fossae. It is a prevalent disease with a significant impact on health-related quality of life (HRQL). Allergies, allergic rhinitis, asthma, and aspirin intolerance are frequently associated. The management is individual. The first line of treatment is long-term treatment with intranasal corticosteroids. Oral corticosteroids should be used with caution. When the medical treatment fails, the patient is eligible for sinus surgery, which usually consists of a complete sphenoethmoidectomy. In the case of symptomatic recurrence after both medical and surgical treatment, biologics are currently a very promising treatment effective on all respiratory tracts. Dupilumab is considered in the literature to be the molecule of choice. However, besides the international guidelines published by EPOS and Euforea, the molecule prescribed depends also on its availability in each country and the criteria edited by the health authorities to receive reimbursement. Traditional medical treatment remains necessary as a complement to biologics. At the moment, there is no consensus on when the medical treatment can be stopped.
Full article

Figure 1
Open AccessArticle
Technical Quality of Contemporary Endoscopic Sinus Surgery: An Assessment by Study of Anatomical Features Needing Attention at Revision Surgery
by
Nitish Kumar, Pedro Lanca Gomes, Michael J. Marino, Amar Miglani and Devyani Lal
Sinusitis 2024, 8(2), 28-36; https://doi.org/10.3390/sinusitis8020005 - 14 Aug 2024
Abstract
►▼
Show Figures
Although technical causes of endoscopic sinus surgery (ESS) failure have long been reported, we were curious about the quality of contemporary sinus surgery. The electronic health database of Mayo Clinic, Arizona was scrutinized to identify adult patients with diffuse chronic rhinosinusitis (CRS) who
[...] Read more.
Although technical causes of endoscopic sinus surgery (ESS) failure have long been reported, we were curious about the quality of contemporary sinus surgery. The electronic health database of Mayo Clinic, Arizona was scrutinized to identify adult patients with diffuse chronic rhinosinusitis (CRS) who underwent revision ESS between January 2019 and September 2023 with a history of bilateral full-house ESS. Anatomical features on preoperative radiology and intraoperative endoscopy were cataloged: residual uncinate tissue, maxillary antrostomy with a non-incorporated natural os, residual ethmoidal septations (three septations > 3 mm), and inadequate sphenoid osteotomy (os size < 6 mm). Sixty-nine subjects were identified. A deviated nasal septum was present in 53.6%. Residual uncinate tissue was noted in 50.7% of patients associated with missed natural maxillary os in 39.13% of antrostomies. An inadequate os diameter was noted in 63.8% of sphenoidotomies. Significant residual septations were seen in posterior ethmoidal cells in 66.7% and anterior ethmoidal cells in 62.3% of patients. Residual frontoethmoidal cells were noted in 72.4% of patients. Although the extent of ESS must be individualized, a high prevalence of features reflecting suboptimal surgery that could limit the success of ESS was identified. These findings merit further consideration for focused training during residency and continuous professional development activities.
Full article

Figure 1
Open AccessArticle
Radiological Assessment of Centrally Limited Sinus Disease in Allergic and Non-Atopic Chronic Rhinosinusitis
by
Ahda Farhah Mohd Kutubudin, Aneeza W. Hamizan, Kew Thean Yean, Farah Dayana Zahedi, Baharudin Abdullah and Salina Husain
Sinusitis 2024, 8(2), 20-27; https://doi.org/10.3390/sinusitis8020004 - 1 Aug 2024
Abstract
Background: A centrally limited radiological pattern, marked by mucosal thickening in the central sinonasal cavity with relatively unaffected surrounding sinuses, has been linked to allergy in chronic rhinosinusitis (CRS). However, a comparison between allergic and non-atopic CRS patients is lacking. The role of
[...] Read more.
Background: A centrally limited radiological pattern, marked by mucosal thickening in the central sinonasal cavity with relatively unaffected surrounding sinuses, has been linked to allergy in chronic rhinosinusitis (CRS). However, a comparison between allergic and non-atopic CRS patients is lacking. The role of anatomical variations in the ostiomeatal complex also remains unclear. Methods: Adult CRS patients with allergic rhinitis, asthma, eczema, and positive allergy tests were recruited. CRS patients without atopic disease and negative allergy tests were controls. CT scans were evaluated for the centrally limited radiologic pattern. Anatomical variations in the ostiomeatal complex were also examined. Results: The study included 15 allergic CRS and 17 non-atopic CRS participants. Allergic CRS patients showed a higher prevalence of centrally limited sinus disease compared to non-atopic CRS patients (50% vs. 14.7%, p < 0.01). No anatomical variations were conclusively linked to allergy status or the centrally limited sinus disease. Conclusion: Centrally limited sinus disease on radiology is associated with underlying allergy in CRS but should not be the primary diagnostic tool. Anatomical variants did not clearly relate to allergy status or the radiologic pattern but this requires further studies.
Full article
Open AccessArticle
Contemporary Update on the Microbiology of Paranasal Sinusitis
by
Margaret B. Mitchell, Alan D. Workman, Richard Lu and Neil Bhattacharyya
Sinusitis 2024, 8(2), 13-19; https://doi.org/10.3390/sinusitis8020003 - 16 Jul 2024
Abstract
Background: Sinusitis, whether acute or chronic, is likely due at least in part to disruptions in the microbiota of the paranasal sinuses. Sinus cultures are often employed to guide medical treatment. Objective: To quantify the contemporary microbiology of the paranasal sinuses and better
[...] Read more.
Background: Sinusitis, whether acute or chronic, is likely due at least in part to disruptions in the microbiota of the paranasal sinuses. Sinus cultures are often employed to guide medical treatment. Objective: To quantify the contemporary microbiology of the paranasal sinuses and better understand the utility of paranasal sinus cultures. Methods: We identified patients from 2018 to 2019 with sinus cultures taken by an otolaryngologist in the outpatient setting in our healthcare system with a concurrent diagnosis of acute or chronic rhinosinusitis. These cultures were analyzed based on their culture type and result. The most commonly isolated bacteria were further analyzed by species; Staphylococcus resistance patterns were analyzed as well. Results: A total of 2302 culture samples were collected: 2012 (87%) bacterial, 287 (13%) fungal, and 3 (0.1%) mycobacterial cultures. The results of more than half (1142, 57%) of these bacterial cultures were positive for a named genus, while those of 592 (29%) were positive for normal sinus flora and 16 (0.8%) for normal oral flora, and those of 183 (9%) showed no growth. The results of another 79 (4%) bacterial cultures were positive for unnamed bacteria, which were not further classified (e.g., Gram-negative rods). Of the positive bacterial cultures with named genera, the most common genera identified was Staphylococcus (383, 34%). Of these, the most common species of Staphylococcus was S. aureus (311, 81%), 42 of which (14%) showed methicillin resistance (MRSA). Of the fungal cultures, 265 (92%) resulted in no growth, and all three mycobacterial cultures showed no growth. Conclusions: In contrast to fungal cultures, the majority (57%) of sinus bacterial cultures showed positive results, with the identification of a named genus, highlighting the potential utility of this assay in guiding medical therapy.
Full article
Open AccessEditorial
Nasal Cytology in Eosinophilic Granulomatosis with Polyangiitis
by
David Longhino, Arianna Aruanno and Eleonora Nucera
Sinusitis 2024, 8(2), 11-12; https://doi.org/10.3390/sinusitis8020002 - 29 Jun 2024
Abstract
In recent years, nasal cytology (NC) has become a valuable diagnostic tool in rhinology due to its easy practicability, non-invasiveness, and low cost [...]
Full article
Open AccessReview
Eosinophilic Cationic Protein and Immunoglobulin E: Unraveling Biomarkers in Chronic Pediatric Cough
by
Snezhina Lazova, Kremena Naydenova and Tsvetelina Velikova
Sinusitis 2024, 8(1), 1-10; https://doi.org/10.3390/sinusitis8010001 - 27 Feb 2024
Abstract
Although the cough reflex is one of the essential protective mechanisms in the respiratory tract, it is considered a considerable health problem in adults and children when it becomes chronic and hypersensitive. However, the need for biomarkers for chronic cough in children and
[...] Read more.
Although the cough reflex is one of the essential protective mechanisms in the respiratory tract, it is considered a considerable health problem in adults and children when it becomes chronic and hypersensitive. However, the need for biomarkers for chronic cough in children and adults is critical. The problem with cough is also a severe symptom in hypersensitivity children. Respiratory infections are a considerable challenge for pediatricians, especially in allergic children. The term cough hypersensitivity syndrome, although introduced in adults, was questioned for children. Eosinophil cationic protein (ECP) is a promising marker for chronic cough but still needs to be validated and proved in clinical settings. In this review article, we aimed to discuss the possible role of ECP in connection to IgE for chronic cough in children.
Full article
Open AccessReview
Chronic Rhinosinusitis with Nasal Polyposis in People with Cystic Fibrosis
by
Jessa E. Miller, Jennifer L. Taylor-Cousar and Daniel M. Beswick
Sinusitis 2023, 7(2), 27-37; https://doi.org/10.3390/sinusitis7020004 - 31 Oct 2023
Cited by 2
Abstract
Cystic fibrosis (CF) is an autosomal recessive disorder that results in deranged ion transport and affects multiple organ systems, including the upper and lower respiratory tracts. People with CF (PwCF) often develop chronic rhinosinusitis (CRS) with or without nasal polyposis. CRS can significantly
[...] Read more.
Cystic fibrosis (CF) is an autosomal recessive disorder that results in deranged ion transport and affects multiple organ systems, including the upper and lower respiratory tracts. People with CF (PwCF) often develop chronic rhinosinusitis (CRS) with or without nasal polyposis. CRS can significantly decrease quality of life for PwCF and can lead to more frequent pulmonary exacerbations. The management of CRS in PwCF is different from that in individuals without CF. Novel therapies have emerged in the last several years that have drastically altered the progression of both pulmonary and sinonasal disease in people with CF. It is critical for providers who manage CF-related CRS to understand the unique characteristics and challenges that coincide with this disease process. This review article aims to provide readers with an overview of the pathophysiology of CF and to summarize best practice strategies for the management of CF-related CRS.
Full article
(This article belongs to the Special Issue Frontiers in Chronic Rhinosinusitis with Nasal Polyposis)
►▼
Show Figures
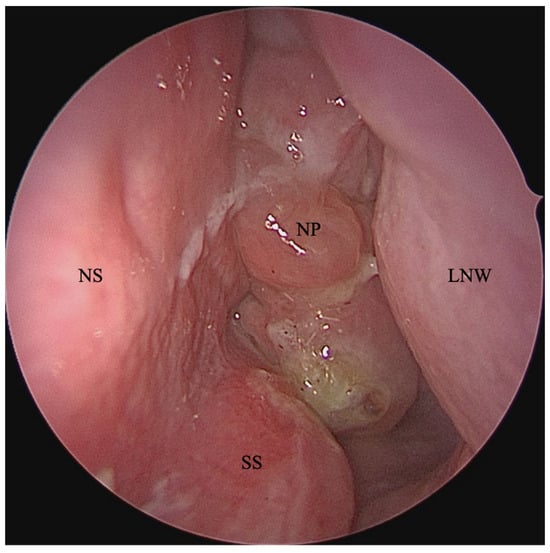
Figure 1
Open AccessReview
Central Compartment Atopic Disease as a Pathophysiologically Distinct Subtype of Chronic Rhinosinusitis: A Scoping Review
by
Camron Davies, Franklin Wu, Emily Y. Huang, Masayoshi Takashima, Nicholas R. Rowan and Omar G. Ahmed
Sinusitis 2023, 7(2), 12-26; https://doi.org/10.3390/sinusitis7020003 - 21 Sep 2023
Cited by 1
Abstract
Central compartment atopic disease (CCAD) is a distinct phenotype within chronic rhinosinusitis with nasal polyps (CRSwNP) with a pathophysiology that bridges the gap between allergy and CRSwNP, an association that was previously ambiguous. Understanding this endotype and its link to allergic disease is
[...] Read more.
Central compartment atopic disease (CCAD) is a distinct phenotype within chronic rhinosinusitis with nasal polyps (CRSwNP) with a pathophysiology that bridges the gap between allergy and CRSwNP, an association that was previously ambiguous. Understanding this endotype and its link to allergic disease is crucial for improved CCAD management. Using a systematic search and an independent dual-reviewer evaluation and data extraction process, this scoping review examines the clinical features, management options, and treatment outcomes of CCAD. Central compartment (CC) polypoid changes of the MT predominantly correlate with allergic rhinitis, increased septal inflammation, oblique MT orientation, and decreased nasal cavity opacification and Lund–Mackay scores compared to other CRSwNP subtypes. CCAD patients also exhibit higher rates of asthma, allergen sensitization, and hyposmia or anosmia. Surgical outcomes, including revision rate and SNOT-22 improvement, are favorable in CCAD as well. In conclusion, CCAD primarily affects atopic individuals and is managed using endoscopic sinus surgery combined with treating the underlying allergy. Continued research is needed to further refine understanding and develop optimal treatment strategies of this emerging CRS subtype.
Full article
(This article belongs to the Special Issue Frontiers in Chronic Rhinosinusitis with Nasal Polyposis)
►▼
Show Figures
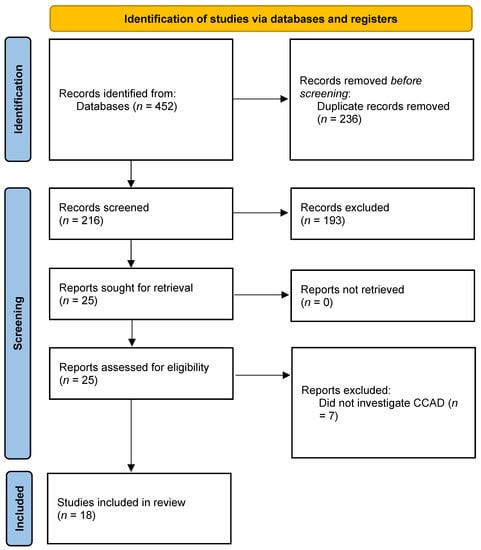
Figure 1
Open AccessCase Report
Bleach-Induced Chemical Sinusitis and Orbital Cellulitis Following Root Canal Treatment
by
Terese Huiying Low, Jun Jie Seah, Somasundaram Subramaniam, Vijayaraj Thirunavukarasu and Chew Lip Ng
Sinusitis 2023, 7(1), 6-11; https://doi.org/10.3390/sinusitis7010002 - 31 May 2023
Abstract
►▼
Show Figures
The authors describe an unusual case of chemical sinusitis and orbital cellulitis secondary to a sodium hypochlorite accident in a patient who had just undergone root canal treatment. The patient presented with acute, progressive symptoms of unilateral maxillary sinusitis, facial cellulitis and orbital
[...] Read more.
The authors describe an unusual case of chemical sinusitis and orbital cellulitis secondary to a sodium hypochlorite accident in a patient who had just undergone root canal treatment. The patient presented with acute, progressive symptoms of unilateral maxillary sinusitis, facial cellulitis and orbital cellulitis which began hours after root canal treatment on the ipsilateral side. He was admitted to hospital under the care of the Otorhinolaryngology team and reviewed regularly by the Ophthalmologists. He underwent Endoscopic Sinus Surgery during his hospital stay. The intraoperative findings revealed necrotic sinus mucosa and slough within the involved maxillary sinus, which were suggestive of chemical burn injury induced by the highly alkaline sodium hypochlorite solution used during root canal treatment. He was treated postoperatively with regular nasal toilet, culture-directed antibiotics and topical ocular pressure-lowering eyedrops. He displayed a slow recovery with eventually no orbital sequelae, but experienced persistent cheek numbness three months post-injury. Severe chemical sinusitis with orbital cellulitis secondary to sodium hypochlorite accident is a rare complication of root canal treatment, with potentially severe consequences. It can present with symptoms similar to complicated acute bacterial sinusitis. Otorhinolaryngologists and dental surgeons should maintain a high index of suspicion when managing a patient post-root canal treatment with symptoms of unilateral sinusitis, facial cellulitis, orbital cellulitis and even airway compromise. This would allow prompt intervention before sight or life-threatening complications set in.
Full article
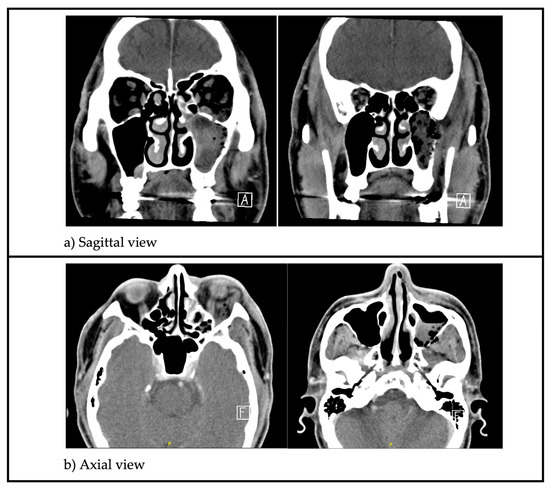
Figure 1
Open AccessBrief Report
Patient-Reported Outcomes with Benralizumab in Patients with Severe Eosinophilic Asthma and Severe Chronic Rhinosinusitis with Nasal Polyps
by
Rory Chan, Kirsten Stewart, Rasads Misirovs and Brian Lipworth
Sinusitis 2023, 7(1), 1-5; https://doi.org/10.3390/sinusitis7010001 - 29 Mar 2023
Cited by 1
Abstract
►▼
Show Figures
Introduction: Chronic rhinosinusitis with nasal polyps (CRSwNP) and severe eosinophilic asthma (SEA) are common comorbidities characterised by type 2 inflammation associated with increased expression of interleukin 5. Methods: Eight patients with SEA and severe CRSwNP attended the Scottish Centre for Respiratory Research as
[...] Read more.
Introduction: Chronic rhinosinusitis with nasal polyps (CRSwNP) and severe eosinophilic asthma (SEA) are common comorbidities characterised by type 2 inflammation associated with increased expression of interleukin 5. Methods: Eight patients with SEA and severe CRSwNP attended the Scottish Centre for Respiratory Research as part of a clinical trial (EudraCT number 2019-003763-22). Following an initial 4-week run-in period (baseline) when patients took their usual inhaled and intranasal corticosteroid treatment for SEA and CRSwNP, they all received subcutaneous benralizumab 30 mg q4w for 12 weeks. Results: Following 12 weeks of benralizumab, no significant differences were detected in nasal global symptom visual analogue score (VAS), hyposmia VAS, total nasal symptom score, or peak nasal inspiratory flow. In contrast, Asthma Control Questionnaire significantly improved along with near-complete depletion of peripheral blood eosinophils by 99%, while eosinophil-derived neurotoxin fell by 72%. Conclusions: Greater improvements in patient-reported outcomes related to asthma were observed than with CRSwNP in response to benralizumab.
Full article

Figure 1
Open AccessArticle
Immunomodulators Containing Epicor, Colostrum, Vitamin D, Zinc, Lactobacilli and Bifidobacterium Reduce Respiratory Exacerbations in Children and Adults with Chronic Pulmonary Diseases
by
Snezhina Lazova, Nikolay Yanev, Nadia Kolarova-Yaneva and Tsvetelina Velikova
Sinusitis 2022, 6(2), 66-76; https://doi.org/10.3390/sinusitis6020009 - 2 Dec 2022
Abstract
(1) Background: A number of studies have demonstrated the connection between developing or exacerbating chronic respiratory diseases in adults and children. However, still, few studies focus on reducing exacerbations via immunomodulation. (2) Methods: In this pilot study, a total of 25 pediatric and
[...] Read more.
(1) Background: A number of studies have demonstrated the connection between developing or exacerbating chronic respiratory diseases in adults and children. However, still, few studies focus on reducing exacerbations via immunomodulation. (2) Methods: In this pilot study, a total of 25 pediatric and adult patients with bronchial asthma (BA) and chronic obstructive pulmonary disease (COPD)/persistent bacterial bronchitis (PBB) were included, administered over-the-counter (OTC) immunomodulators and followed up for 6 or 12 months. (3) Results: We observed a decrease in the frequency of exacerbations with slight improvements in functional respiratory indicators in adults on their second and third visits and a reduced number of exacerbations and improved spirometry indices in children with BA, although exacerbations requiring hospital admission remained at a similar rate. (4) Conclusions: We confirmed that the number of exacerbations of underlying chronic respiratory disease in adults and children could be reduced after the administration of OTC immunomodulators, probably by optimizing the immune resistance to common viral infections.
Full article
(This article belongs to the Special Issue Feature Papers in Sinusitis 2022)
►▼
Show Figures

Figure 1
Open AccessArticle
The Safety of Topical and Intravenous Tranexamic Acid in Endoscopic Sinus Surgery
by
Agrani Ratnayake Kumar and Andrew James Wood
Sinusitis 2022, 6(2), 56-65; https://doi.org/10.3390/sinusitis6020008 - 18 Oct 2022
Abstract
Tranexamic acid (TXA) is an inexpensive and widely used medication indicated for the reduction of bleeding. There are data showing the efficacy of intravenous (IV) and topical TXA in endoscopic sinus surgery (ESS) but the safety of this practice is not well studied.
[...] Read more.
Tranexamic acid (TXA) is an inexpensive and widely used medication indicated for the reduction of bleeding. There are data showing the efficacy of intravenous (IV) and topical TXA in endoscopic sinus surgery (ESS) but the safety of this practice is not well studied. The objective of this study was to assess the safety of using both IV and topical TXA in ESS. A scoping review was performed to investigate the effect of TXA on respiratory epithelia. A retrospective single-surgeon study was used to assess 177 comprehensive ESS cases from January 2017–December 2019 for the safety of combined IV and topical TXA. The scoping review demonstrated that respiratory epithelia could withstand a wide range of TXA concentrations without detrimental morphological effects. Topical TXA may have positive effects on wound healing and inflammation. The retrospective study showed no thromboembolic complications attributable to TXA in the 28 days after ESS. Only two patients (1.3%) who received TXA re-presented with post-operative bleeding. The use of IV and topical TXA is safe with regards to its effect on respiratory epithelium and thromboembolic disease. Topical TXA may have more positive effects than merely the reduction of bleeding following ESS.
Full article
(This article belongs to the Special Issue Innovations in the Management of Chronic Rhinosinusitis)
►▼
Show Figures
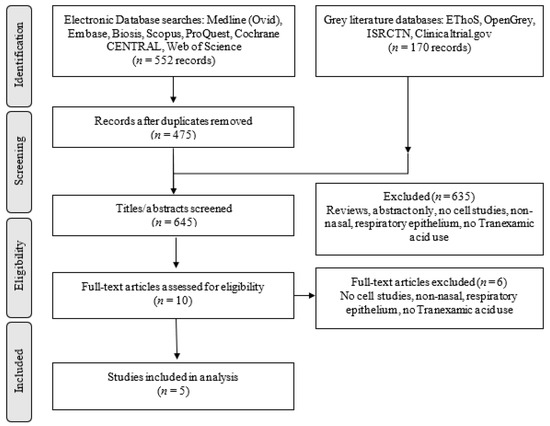
Figure 1
Open AccessReview
Home-Based Respiratory Care for COPD Patients
by
Ricardo G. Figueiredo, Caio Laudano, Jaqueline Muniz and José de Bessa, Jr.
Sinusitis 2022, 6(2), 49-55; https://doi.org/10.3390/sinusitis6020007 - 12 Sep 2022
Cited by 1
Abstract
Despite significant advances in pharmacological treatment over the last few decades, COPD remains a heavy burden on the health systems around the world, affecting approximately 210 million people, with elevated morbimortality and socioeconomic impact. Barriers to healthcare access were even more evident during
[...] Read more.
Despite significant advances in pharmacological treatment over the last few decades, COPD remains a heavy burden on the health systems around the world, affecting approximately 210 million people, with elevated morbimortality and socioeconomic impact. Barriers to healthcare access were even more evident during the coronavirus disease 19 (COVID-19) pandemic and increased patients’ vulnerability to physical deconditioning, depression, and social isolation. Home-based respiratory care in patients with COPD provides a valuable contribution to effective disease management, with potential advantages for monitoring, treatment adherence, and cost reduction. Technological innovation allows clinical markers of interest, such as respiratory frequency, pulmonary function, and oxygen saturation, to be tracked remotely from the patients’ homes, providing a better understanding of their real needs. Home-based telerehabilitation can also be a viable alternative to hospital-based programs. Here, we highlight the full extent of health benefits of HRC in COPD, particularly for patients with a higher risk of exacerbations, multiple comorbidities, and limited access to health services.
Full article
(This article belongs to the Special Issue The Asthma, Rhinitis and Chronic Pulmonary Diseases)
►▼
Show Figures
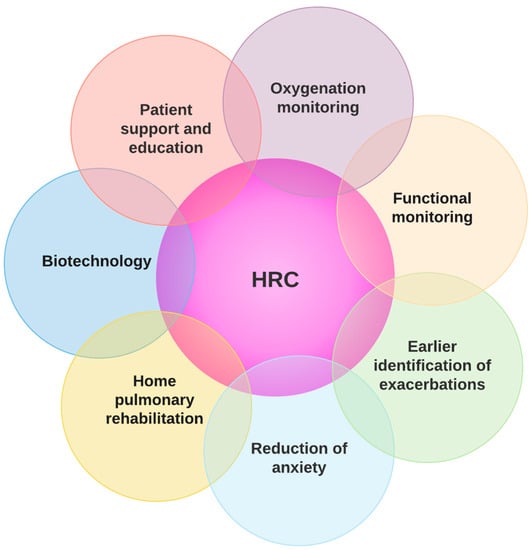
Figure 1
Open AccessArticle
Recurrent Acute Otitis Media Could Be Related to the Pro-Inflammatory State That Causes an Incorrect Diet
by
Fernando M. Calatayud-Sáez, Blanca Calatayud and Ana Calatayud
Sinusitis 2022, 6(2), 36-48; https://doi.org/10.3390/sinusitis6020006 - 22 Aug 2022
Cited by 4
Abstract
Introduction: Acute Otitis Media (AOM) is the most commonly-occurring bacterial complication in childhood. After making certain corrections to the patients’ dietary habits, which we found to be excessively high in animal-based and industrially-processed foods, we observed a significant reduction in recurrent colds and
[...] Read more.
Introduction: Acute Otitis Media (AOM) is the most commonly-occurring bacterial complication in childhood. After making certain corrections to the patients’ dietary habits, which we found to be excessively high in animal-based and industrially-processed foods, we observed a significant reduction in recurrent colds and their bacterial complications. We promote an original way of treating these diseases, since until now the conventional treatment is based on pharmacological and surgical treatment. From our point of view, the mucosa that covers the entire ENT area is in a pro-inflammatory and hyper-reactive state, as a consequence of the alterations produced by an inadequate diet. For us there is no difference in the nutritional treatment of the different mucous membranes that cover the ENT area. The purpose of the study was to assess the effects of the Traditional Mediterranean Diet (TMD) on patients diagnosed with Recurring Acute Otitis Media (RAOM). Methods: prospective pre-postest comparison study with 48 girls and 42 boys aged 1–5 years, each of whom had been and included on the 1-year programme “Learning to eat the Mediterranean Way”, designed to encourage the adoption of the TMD. We studied clinical and therapeutic variables and various anthropometric parameters. Results: all the symptomatic indicators studied (number and intensity of episodes of otitis and emergency admissions) showed a positive and statistically significant evolution in RAOM. By the end of the study, none of the patients met the criteria for classification as RAOM, and 60% percent of patients did not present any further episodes of AOM. In line with the above, the use of anti-microbial drugs and symptomatic treatments reduced considerably; the use of antibiotics dropped from 4.30 occasions/patient/year, to 0.66 (p < 0.001), and the used of symptomatic treatments dropped from 7.63 to 2.75 (p < 0.001). The level of family satisfaction was very high. Conclusions: the adoption of the Traditional Mediterranean Diet has been demonstrated to significantly reduce occurrence of acute otitis media and may contribute to the treatment of patients diagnosed with recurrent acute otitis media.
Full article
(This article belongs to the Special Issue Rhinosinusitis, Otitis, Tubaritis, Adenoiditis, and Other Inflammatory Diseases (-Itis), Mediated by Immunological Alterations Caused by Inadequate Nutrition)
►▼
Show Figures
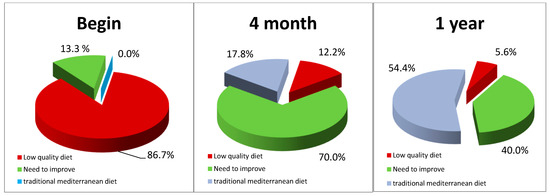
Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics





