Treatment of Hepatocellular Carcinoma and Cholangiocarcinoma
A topical collection in Cancers (ISSN 2072-6694). This collection belongs to the section "Cancer Therapy".
Viewed by 74316Editor
Interests: cholangiocarcinoma; role in vascular and hepatobiliary diagnostic and interventional procedures
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
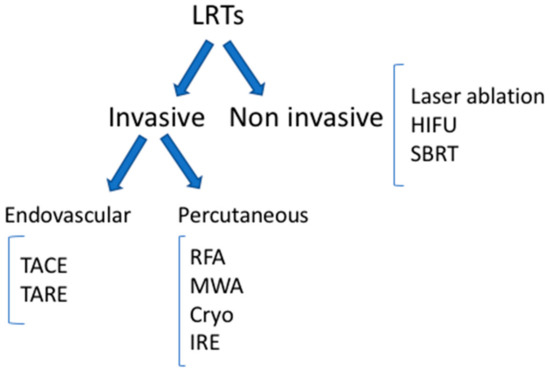
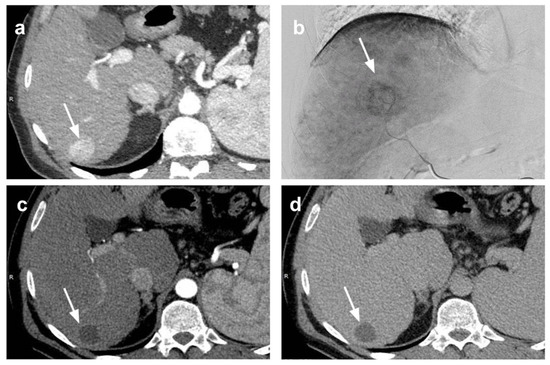
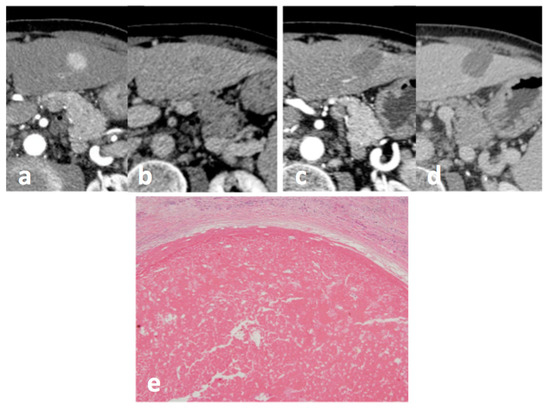
In this Topical Collection are summarized the current indications to different therapeutic options for hepatocellular carcinoma (HCC) and cholangiocarcinoma and more recent results are presented, according to the technologic advancements acquired in recent years. Novel treatment options for patients with HCC and cholangiocarcinoma have been introduced in the last few years, including percutaneous therapies, such as microwave ablation, cryoablation, and intra-arterial treatments such as drug-eluting bead chemoembolization, balloon-assisted chemoembolization, and radioembolization. The most advanced surgical approaches are also described. Systemic therapy of both tumors is also presented, with a special focus on immunotherapy. Advanced imaging analysis, such as radiomics, is presented, which can help in better evaluating the response to therapy and, therefore, allowing a better patient selection.
Dr. Cristina Mosconi
Collection Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Cancers is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2900 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- liver tumors
- interventional treatments
- systemic treatment
- surgery
- response evaluation
- radiomics