Stem Cell-Based Therapy, Disease Modeling and Drug Discovery
A topical collection in Cells (ISSN 2073-4409). This collection belongs to the section "Stem Cells".
Viewed by 74876Editor
Interests: stem cells; tissue regeneration; cell protection; disease modeling; mitochondria; non-coding RNAs
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
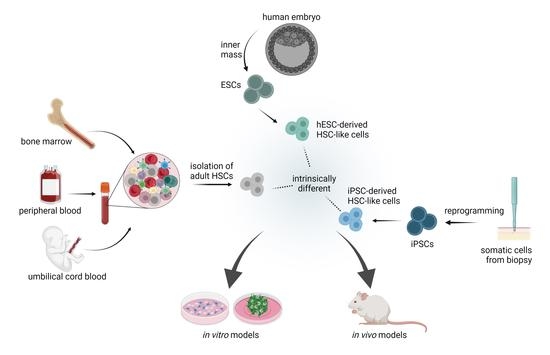
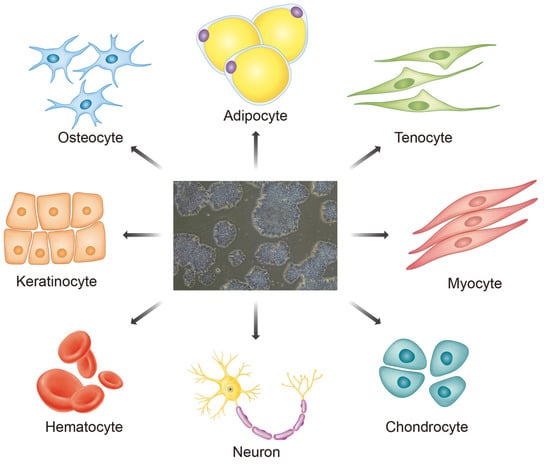
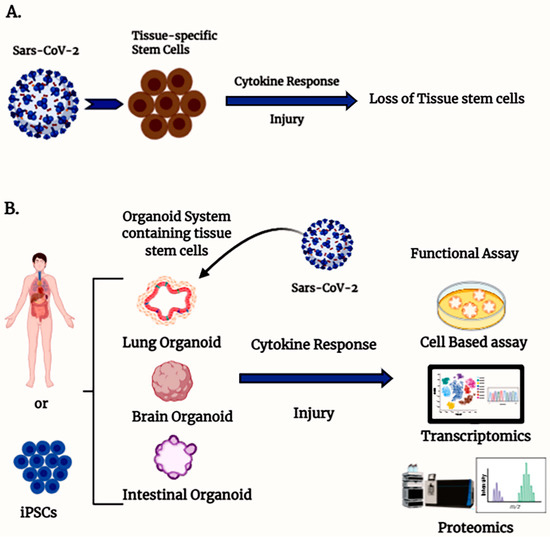
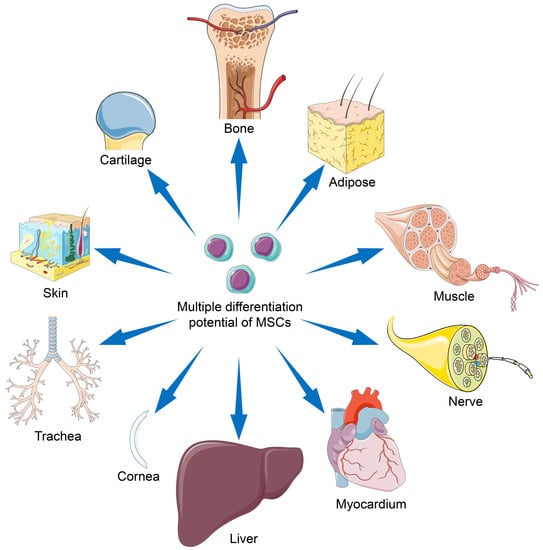
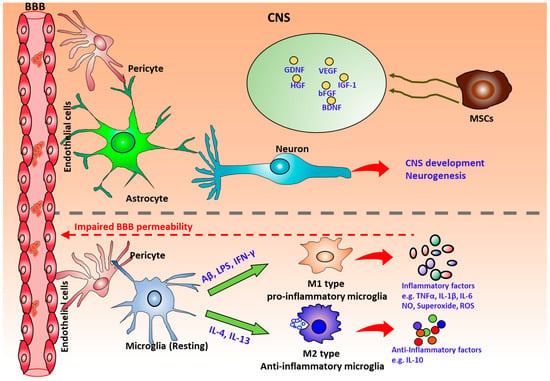
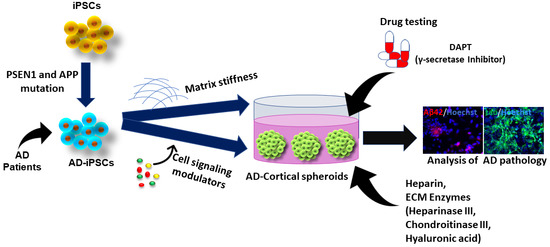
Regenerative cell therapy has the potential to heal or replace tissues and organs damaged by age, disease, or injury. Stem cells represent a great promise as a cell source for regenerative cell therapy and have received increasing attention from basic scientists, clinicians, and the public due to their self-renewing capacity and the ability to form multiple cell types. Stem cells are present in the human body at all stages of life, from the earliest times of development (e.g., embryonic stem cells and fetal stem cells) through adulthood (various adult stem cells). Different types of stem cells differ in the aspects of proliferation and differentiation, which results in their various potential applications in cell therapy. Induced pluripotent stem cells (iPSCs) can be reprogrammed from somatic cells such as skin and blood cells into embryonic stem cell-like pluripotent cells with the ability to generate an unlimited type of human cells, as needed for therapeutic purposes. Additionally, human stem cells with their differentiation potential constitute a promising system for disease modeling. In particular, recent progress in the field of cellular reprogramming has opened the doors to a new era of disease modelling. In fact, iPSCs can be generated from diverse patient populations, expanded, and differentiated into a disease-related cells (e.g., neurons and blood cells), which can then be used as a tool to improve the understanding of disease mechanisms and test therapeutic interventions. This Topical Collection will present state-of-the-art research of stem cell-based therapy, drug discovery and disease modeling. We anticipate that this volume will establish a new benchmark for the refinement of new technologies for reprogramming cells as well as for our understanding of stem cell differentiation, stem cell-based tissue regeneration potential, disease mechanisms, and efficacy and toxicity of drugs. In this Topical Collection, we are seeking high-quality reviews, research papers, case reports, letters to the Editor, editorials, and technical reports on the following topics related to stem cell biology, stem cell-based therapy, drug discovery, and disease modeling:
- Stem cell-based therapy and disease modeling
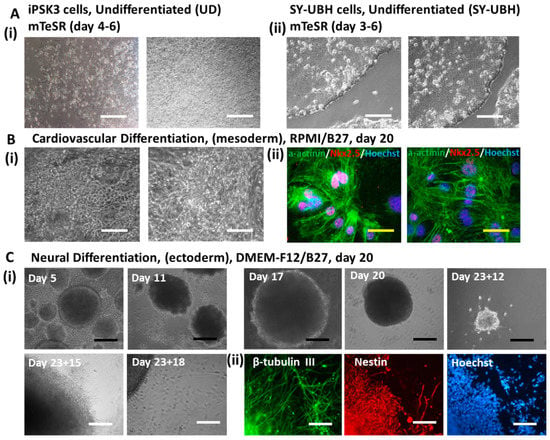
- Stem cell differentiation approaches and mechanisms
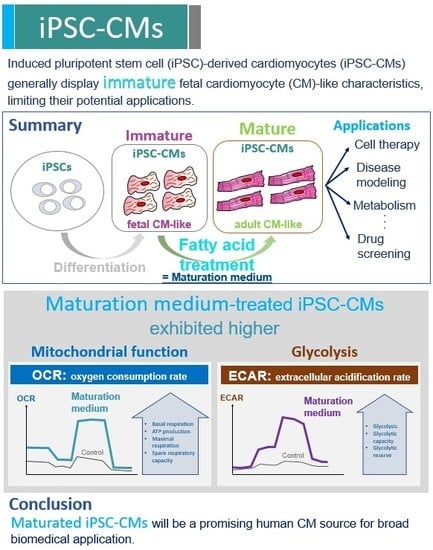
- Maturation of stem cell-derived somatic cells (e.g., neurons and cardiomyocytes)
- Mechanisms (e.g., exosome and microRNAs) of stem cell-mediated tissue regeneration
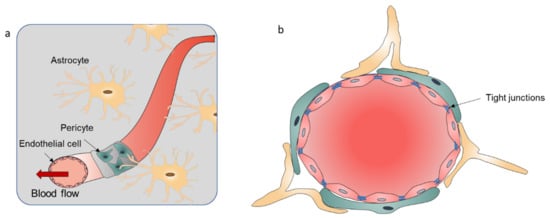
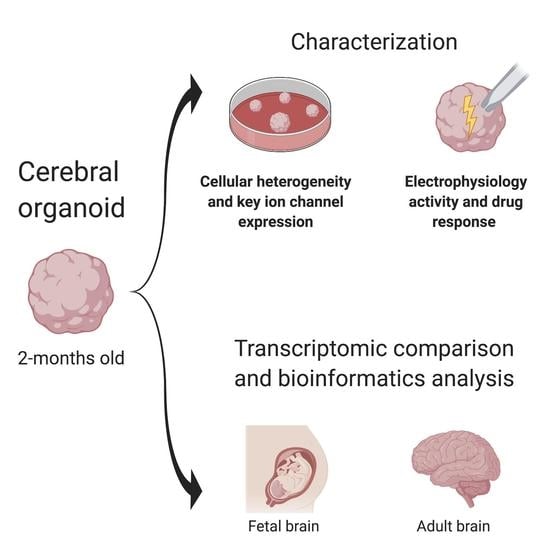
- 3D organoid models and 3D-printed tissues
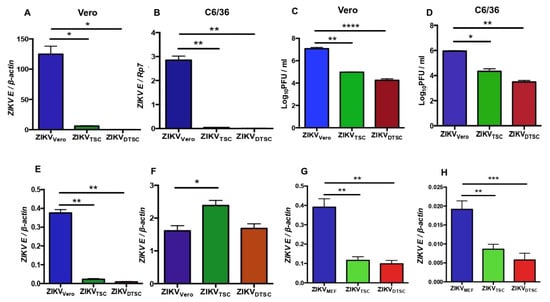
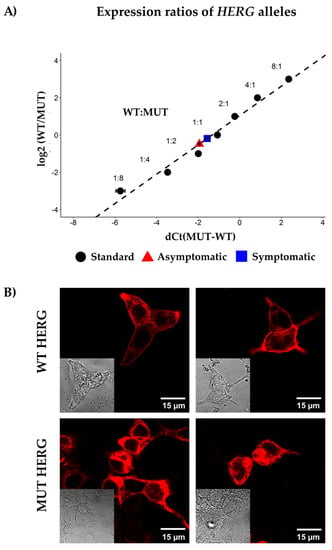
- Stem cell-based drug screening for toxicity and efficacy
- Stem cell-based precision medicine
Prof. Xiaowen Bai
Collection Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Cells is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2700 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- adult stem cells
- induced pluripotent stem cells
- embryonic stem cells
- tissue regeneration
- disease modeling
- paracrine effect
- tissue engineering
- 3D organoids
- cell proliferation and differentiation
- 3D-printed tissues
- drug screening
Related Special Issue
- Stem Cell-based Therapy and Disease Modeling in Cells (22 articles - displayed below)